Eating Disorders and Substance Use
Substance use and substance use disorders (SUD) can often co-occur with eating disorders. Both SUDs and eating disorders are complex conditions associated with significant mental, physical, and social complications. Research suggests that the lifetime prevalence of co-occuring substance use disorder in people experiencing an eating disorder is approximately 21.9% (1).
Eating disorders
Eating disorders are serious mental illnesses characterised by disturbances in behaviours, thoughts and feelings towards body weight and shape, and/
or food and eating. Eating disorders are common and their prevalence is increasing. More than one million Australians are currently experiencing an eating disorder (2). Of people experiencing an eating disorder, 3% have anorexia nervosa, 12% have bulimia nervosa, 47% have BED and 38% have other eating disorders (2).
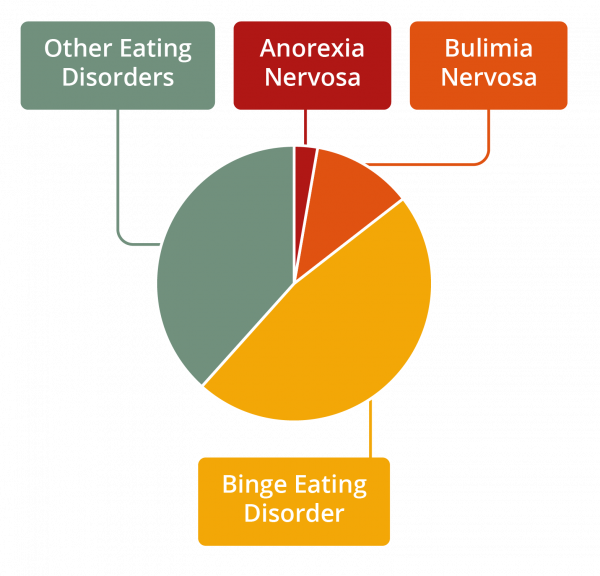
Figure 1: Prevalence of eating disorders by diagnosis
Substance use
Substance use is a broad term that refers to the use or misuse of alcohol, psychoactive drugs (over the counter, prescription and illicit) and other addictive substances (such as tobacco and caffeine). Substances may be used by people for various reasons, including to alter emotional, physical and psychological functioning and experiences, such as (3):
• Increasing energy
• Regulating mood
• Self-medicating
• Relieving physical pain
• Coping with difficult emotions e.g., grief, stress
• Coping with difficult situations e.g., financial stress, relationship stress
• Boosting social confidence
• Peer pressure to fit in
• Weight loss
• Curiosity, experimentation or rebellion
Substance use disorder
A substance use disorder (SUD) occurs when the use of substances becomes excessive, unmanageable, is distressing, and is impacting significantly on a person’s ability to engage in life. Approximately 3.3% of Australians are experiencing a substance use disorder in any given year (4).
The Diagnostic and Statistical Manual of Mental Disorders (DSM) outlines 11 criteria for substance use disorders, with criteria falling under four groupings: impaired control, social impairment, hazardous use, and physical changes (5).
The criteria listed for substance use disorder in the DSM-5 include:
• Taking the substance in larger amounts or for longer than you are meant to
• Wanting to cut down or stop using the substance but not managing to
• Spending a lot of time getting, using, or recovering from use of the substance
• Cravings and urges to use the substance
• Not managing to do what you should at work, home, or school because of substance use
• Continuing to use, even when it causes problems in relationships
• Giving up important social, occupational, or recreational activities because of substance use
• Using substances again and again, even when it puts you in danger
• Continuing to use, even when you know you have a physical or psychological problem that could have been caused or made worse by the substance
• Needing more of the substance to get the effect you want (tolerance)
• Development of withdrawal symptoms, which can be relieved by taking more of the substance
The essential feature of a substance use disorder is a collection of mental, physical and behavioral symptoms indicating that the person continues using the substance despite significant related problems (5).
Impacts and consequences
Both SUDs and eating disorders can cause complex emotional, physical, and social complications which can negatively impact a person’s health and quality of life. When these conditions are experienced concurrently, it can result in even poorer outcomes.
People with eating disorders who also have a SUD tend to have a more severe eating disorder and SUD symptoms, have higher relapse rates, have more severe medical complications, and are more functionally impaired than people with eating disorders alone (8, 9, 10). Both eating disorders and SUDs can lead to death; research suggests that when combined the mortality rate is even greater than the mortality rate for each alone (6, 7, 9).
Warning signs
The warning signs of a co-occurring eating disorder and SUD can be physical, psychological, and behavioural. It is possible for a person to display a combination of these symptoms, or no obvious symptoms at all.
Presentation of signs and symptoms will vary between people and between different diagnoses.
Warning signs for eating disorders:
Physiological
• Sudden changes or fluctuations in weight
• Signs of frequent vomiting e.g., swollen cheeks, calluses on knuckles, damage to teeth
• Fainting or dizziness
• Fatigue
• Hormonal changes e.g., menstrual irregularities, low libido
• Gastrointestinal complaints
• Sleeping problems
• Impaired immune functioning
Psychological:
• Preoccupation with eating, food, body shape or weight
• Low self-esteem
• Feelings of shame, self-loathing or guilt
• Body dissatisfaction and poor body image
• Mood fluctuations
• Heightened anxiety or irritability
• Depression or anxiety
• Self-harm or suicidality
Behavioural:
• Changes to eating habits and behaviours
• Restrictive dieting or patterns of binge eating
• Compulsive exercising
• Wearing loose fitting clothing
• Going to the bathroom during or after meals
• Secretive behaviours around food and/or exercise
• Withdrawal from social activities, particularly those that involve food
• Obsessively and repetitively weighing themselves or body checking
Warning signs for substance use disorder:
Physiological
• Changes in appetite and sleep patterns
• Nutritional deficiencies and weight fluctuations
• Withdrawal symptoms e.g., agitation, irritability, disturbed sleep, dizziness, nausea, sweats/chills, tremors
• Lack of energy
• Oral ill-health
Psychological:
• Depression and anxiety
• Low self-esteem
• Low motivation
• Irritability, agitation and mood swings
• Difficulty concentrating
• Difficulty planning and organising daily activities
• Recurring preoccupation / craving for substance use
Behavioural:
• Evidence of repetitive and hazardous use of substances
• Dramatic changes in daily habits and/or priorities
• Changes in attitudes / personality
• Changes in self-care
• Changes in social behaviour or social network, social isolation
• Engaging in secretive behaviour
• Decrease in performance or not meeting obligations or responsibilities
• Engaging in aggressive or risky behaviour
Causes and risk factors
Substance use challenges may begin before or during an eating disorder, or even after recovery. It is not yet known whether one disorder replaces or provides cover for the other, whether one drives the other, or whether they might co-occur coincidentally. It is likely that this will vary from person to person.
The elements that contribute to the development of these disorders are complex, and involve a range of biological, psychological, and sociocultural factors. However, there are some shared risk factors for both disorders.
Shared risk factors for both SUDs and eating disorders include (8, 10):
• Genetics
• Brain function
• Family history of either condition
• Low self-esteem
• Co-occurring depression and anxiety
• Past experiences of trauma or abuse
• Social pressures
• Tendency to engage in compulsive or impulsive behavior
• Social isolation
• Difficulty regulating mood or emotions
Recovery
Recovery from co-occurring SUDs and eating disorders is possible. If you (or someone you know) is experiencing symptoms of an eating disorder and/or substance use disorders, remember that you are not alone and there are many treatment and support options available. The path to recovery can be long and challenging, however, with the right team and support, it is possible.
Treatment
Where possible, eating disorders and SUDs should be treated simultaneously and by professionals who specialise in both SUDs and eating disorders (8, 10).
Treatment will vary depending on the needs of the person but will generally involve a multidisciplinary team of health professionals. At a minimum, the treatment team for a person experiencing an eating disorder should consist of a medical practitioner and a mental health professional, with a dietitian’s involvement where necessary. In cases of co-occurrence, such as a co-occurring SUD, other health and medical professionals may be required to support the person and address each part of the illness. These may include a GP, alcohol and other drug (AOD) worker, psychiatrists, social worker, and lived experience workers (please see further information on the care team here).
At the centre of any care team is the person experiencing the disorder, and their family and supports. Treatment plans should always be developed within a person-centred, family and culture-sensitive and recovery-oriented framework, and thus information and decision making is shared between all members of the care team.
Treatment approaches may consist of a combination of the following (8, 10, 11):
• Medical treatment e.g., medical stabilisation and withdrawal management
• Therapy or counselling
• Psychoeducation
• Relapse prevention
• Nutrition support
• Medications
• Occupational therapy
• Complementary or alternative therapies e.g., art therapy, music therapy, peer support and social support groups, community-based interventions, etc.
Getting help
If you think that you or someone you know may have an eating disorder with or without a co-occurring SUD, it is important to seek help immediately. The earlier you seek help the closer you are to recovery. Your GP is a good ‘first base’ to seek support and access eating disorder and/or substance use treatment.
To find help in your local area go to NEDC Service Locator.
Find information about helplines via our Get Help page.
Download Eating Disorders and Substance Use fact sheet here.
References
1. Bahji A, Mazhar MN, Hudson CC, Nadkarni P, MacNeil BA, Hawken E. Prevalence of substance use disorder comorbidity among individuals with eating
disorders: A systematic review and meta-analysis. Psychiatry Research. 2019 Mar;273:58–66.
2. Deloitte Access Economics. (2012). Paying the price: the economic and social impact of eating disorders in Australia.
3. Alcohol and Drug Foundation. Why do people use alcohol and other drugs? [Internet]. ADF; 2021
4. Australian Bureau of Statistics. National Study of Mental Health and Wellbeing, 2020-21. ABS; 2022.
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed, text revision. 2022.
6. Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies.
Archives of general psychiatry. 2011 Jul;68(7):724–31.
7. Preti A, Rocchi MBL, Sisti D, Camboni MV, Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatrica
Scandinavica. 2010 Nov 24;124(1):6–17.
8. Gregorowski C, Seedat S, Jordaan GP. A clinical approach to the assessment and management of co-morbid eating disorders and substance use
disorders. BMC Psychiatry. 2013 Nov 7;13(1).
9. Eating Disorders Review. Substance Use Disorders and Eating Disorders [Internet]. Eating Disorders Review; 2021.
10. Kanbur N, Harrison A. Co-occurrence of Substance Use and Eating Disorders: An Approach to the Adolescent Patient in the Context of Family Centered
Care. A Literature Review. Substance Use & Misuse. 2016 Apr 20;51(7):853–60.
11. National Institute of Mental Health. Substance Use and Co-occurring Mental Disorders. NIMH; 2021.

