The National Eating Disorders Strategy 2023-2033 provides a clear roadmap to guide sector development and policy decision-making for the next decade. It is the culmination of extensive consultation and review, and sets a shared direction for the sector and the broader system of care. The National Strategy was developed by NEDC, with funding from the Australian Government Department of Health and Aged Care.
The National Strategy articulates the key components, standards and actions that are required to achieve an effective, equitable and coordinated system of care, and the roles of different stakeholders. Implementation of the National Strategy will help to achieve evidence-based national consistency, and ensure that people experiencing or at risk of eating disorders, and their families/supports and communities can access the care that they need, when they need it.
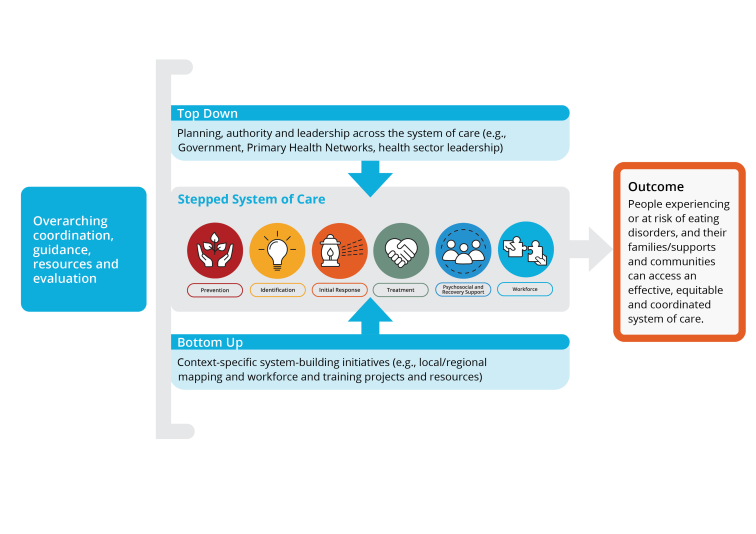
National Strategy Implementation Model
Successful implementation of the National Strategy will require 'top-down' planning, authority and leadership across the system of care, in conjunction with 'bottom-up' context-specific system-building initiatives. It will also require overarching coordination, guidance, resources, and evaluation, to help to drive change, maximise impact, and reduce duplication.
You can download a full page copy of the overarching framework here.
Coordination of National Strategy implementation will be led by NEDC.
Principles of implementation
Implementation of the National Strategy will be underpinned by the following principles:
Lived experience guidance leadership: The expertise and insights of people who are experiencing or who have experienced an eating disorder and their families/supports and communities are central in decision-making, design, and evaluation of implementation activities
Partnerships and collaboration: Foster strong, cross-sectoral partnerships across government, eating disorders, health and mental health sectors, community, jurisdictions, disciplines, and lived experience to drive coordinated action
Cross-promotion and non-duplication: Align efforts across stakeholders, leveraging existing resources and initiatives to avoid fragmentation and inefficiencies
Relationship building and trust: Invest in long-term relationships across the sector to strengthen shared commitment, communication, and system-wide accountability
System integration and whole-of-system thinking: Ensure that actions reinforce a seamless system of care, thought integrating and interconnections between the components of the system of care and reinforce the broader system rather than operate in isolation
Equity and accessibility: Prioritise approaches that address disparities in access to care, ensuring services are inclusive, culturally safe, and responsive to diverse needs
Data-driven decision making and evidence generation: Use evidence, implementation research, and continuous evaluation to guide actions, measure progress, and adjust strategies. Report on outcomes to enhance the evidence base and drive ongoing change
Scalability and sustainability: Design implementation efforts with long-term sustainability in mind, embedding new practices into policy, funding models, and workforce capacity
Flexibility and adaptability: Recognise that implementation occurs in dynamic environments; be responsive to emerging challenges, opportunities, and feedback
Clear governance and accountability: Establish transparent structures for oversight, reporting, and shared responsibility to maintain momentum and ensure progress
Implementation phases
Sustainable change takes time, and the process of National Strategy implementation will occur across three main phases:
1. Activation phase 2023-2027: This phase focuses on initiating implementation by establishing foundational structures, building stakeholder engagement, and mobilising resources to support early progress against priority targets
2. Integration phase 2027-2030: In this phase, Priority Actions are embedded into existing systems and services, strengthening coordination and ensuring consistency in practice across the system of care. Simultaneously, priority levers for the second period are implemented in collaboration with stakeholders.
3. Sustainability phase 2030-2033: This phase ensures long-term impact by securing ongoing resourcing, embedding continuous improvement processes, and reinforcing policy and system-level supports to maintain and evolve the established system of care.
Research and evaluation
Over the 10-year implementation of the National Strategy, NEDC will support evidence-to-practice translation in eating disorder systems change across Australia. We will apply best-practice evidence in implementation, change management, and eating disorder care while continuously evaluating and sharing findings to strengthen the evidence base through research and academic partnerships.
NEDC is committed to highlighting workforce and service development innovations driving systems change. Our approach to evaluation is detailed in the National Strategy Evaluation Framework.
You can read more about National Strategy Evaluation here.
Priority levers for implementing the National Strategy (2023-2027)
Based on the three key drivers for systems-based change outlined in NEDC’s National Strategy Implementation Model (top-down, bottom-up, overarching coordination), consultation with key stakeholders, research review and gap analysis, three key levers have been identified to activate broad and sustainable implementation of the National Strategy.
These priority levers will help to achieve early change towards the Strategy’s desired outcomes for people with lived experience and their families/supports and communities and lay the foundation for effective action across the subsequent phases of National Strategy implementation. These levers ensure coordinated, strategic approaches by all stakeholders, which will maximise impact and reduce duplication.
Acknowledging the required support from government, the eating disorder sector, health, mental health and psychosocial support organisations, and community, several proposed activities are outlined within each lever to facilitate the achievement of these outcomes over year 1-4 of National Strategy implementation. These are outlined below.
1. Activate national and jurisdictional planning and coordination
2. Kickstart sustainable local/regional system-building across Australia
3. Increase workforce capacity to respond to eating disorders, disordered eating and body image concerns
Priority levers - Activities
✔ Overarching coordination – NEDC is leading a national, structured effort to guide implementation across jurisdictions, ensuring consistency while allowing for tailored local solutions. We are working closely with governments, professional bodies, service providers, service development and lived experience organisations to align efforts and embed best practices.
✔ Stakeholder activation – The success of this Strategy depends on the engagement and leadership of stakeholders at all levels. We are working with sector leaders—including health professionals, policy-makers, and community organisations—to drive practical changes within their own spheres of influence. Through National Implementation Network meetings, sprint groups, and targeted initiatives, we are ensuring that the right people are involved at the right time.
✔ Strategic communication & resources – To support implementation, we are providing a suite of practical resources, including the My Action Plan tool, professional development databases, and targeted training materials for different workforce groups. The National Strategy Action Hub has been launched as a centralised space for tracking actions, accessing resources, and sharing updates.
✔ Bottom-up initiatives – NEDC is leading some bottom-up initiatives as aligned with National Strategy Actions. This includes:
- The development of the Eating Disorder Safe principles and ongoing consultation and support to support their rollout across community
- Embedding eating disorder content in tertiary curricula for medicine, psychiatry, psychology, nursing, occupational therapy, social work, and dietetics
- Primary Health Network (PHN) collaborations to embed eating disorder expertise in primary care.
- Targeted initiatives for underserved populations, including Aboriginal and Torres Strait Islander communities, neurodivergent individuals, people with longstanding eating disorders, and people with higher weight.
- Workforce development strategies to enhance training, supervision, and support for professionals across disciplines
- Leading the Right Care, Right Place project, seeking to establish a more accessible and integrated system of care through the introduction of an Eating Disorder Coordinator model within four distinct PHNs
National Strategy Implementation Network
NEDC has convened a National Strategy Implementation Network, with members from every state and territory, from all eating disorder lived experience and service development organisations, and representing key system-building perspectives. The purpose of the Implementation Network is to provide strategic advice on National Strategy implementation, and to help champion implementation initiatives.
Implementation Network members:
| Dr June Alexander | Lived Experience Advocate and Mentor |
| Professor Leah Brennan | La Trobe University; Centre for Eating, Weight and Body Image |
| Dr Susan Byrne | University of Western Australia |
| Belinda Caldwell | Eating Disorders Victoria |
| Shannon Calvert | Lived Experience Educator; Advisory Consultant |
| Gillian Chat | Department of Health, Northern Territory |
| Belinda Chelius | Eating Disorders Queensland |
| Laurence Cobbaert | Eating Disorders Neurodiversity Australia |
| Rebecca Creek | Department of Health, Northern Territory |
| Gemma Davis | WA Mental Health Commission |
| Dr Anthea Fursland | Clinical Psychologist |
| Jade Gooding | Australia and New Zealand Academy of Eating Disorders |
| Amy Hannigan | Queensland Eating Disorder Service |
| Kellie Horton | Department of Health, Victoria |
| Jim Hungerford | Butterfly Foundation |
| Neema Jose | ACT Eating Disorders Service |
| Rachel Knight | Deakin University and Western Health |
| Dr Randall Long | Statewide Eating Disorder Service South Australia |
| Peta Marks | Australian Eating Disorders Research and Translation Centre; InsideOut Institute |
| Andy McGregor | South Australia Statewide Eating Disorders Service (SEDS) |
| Thy Meddick | Qld CYMHS, Eating Disorders Team |
| Louella Monoghan | WA Mental Health Commission |
| Fintan O'Looney | WA Eating Disorders Outreach and Consultation Service (WAEDOCS) |
| Gise Paine | Department of Health, South Australia |
| Anita Reimann | Tasmanian Eating Disorder Service (TEDS) |
| Michelle Roberton | Victorian Centre of Excellence in Eating Disorders (CEED) |
| Jane Rowan | Eating Disorders Families Australia (EDFA) |
| Madeleine Sewell | CAMHS Eating Disorder Service, Perth Children’s Hospital |
| Dr Andrew Wallis | SCHN Eating Disorder Service Network |
| Sharon Ward | Department of Health, Queensland |
| Dr Zali Yager | The Embrace Collective |
| Sharnae Zanotti | WA Mental Health Commission |
| Dr Sarah Trobe | NEDC National Director |
| Dr Sarah Giles | NEDC Research and Evaluation Lead |
| Louise Dougherty | NEDC Strategy and Policy Lead |
Further information
This page contains links to National Strategy implementation events and resources, and will continue to be added to over time.
If you have any questions about National Strategy implementation or need support with your own local plan, please email nationalstrategy@nedc.com.au
How to access the National Eating Disorders Strategy 2023-2033
You can access the full Strategy here.
You can use the main landing page for the National Strategy to navigate to other resources and information.

