Eating disorders are serious, complex mental illnesses accompanied by physical and mental health complications which may be severe and life threatening. They are characterised by disturbances in behaviours, thoughts and feelings towards body weight and shape, and/or food and eating.
People experiencing or at risk of an eating disorder, and their families/supports and communities may require access to a range of different services, at different levels of intensity or frequency, across the course of illness (or risk of illness) and recovery. Coordinated, evidence-based services that are matched to a person's needs, and which increase or decrease in intensity according to a person’s changing psychological, physical, nutritional and psychosocial needs are known as the ‘stepped system of care’ for eating disorders. Progression along the continuum is not linear, and a person may require recurrent episodes of treatment and support, at different levels in the stepped system of care and from different services providers.
NEDC has developed a model which depicts the components of the stepped system of care for eating disorders, with examples of contexts where these components may be delivered (shown below). Principles and guidelines, lived experience, and research and evaluation should underpin and inform all components. Similarly, involvement of the person experiencing or at risk of an eating disorders and their family/supports and community is integral across the stepped system of care.
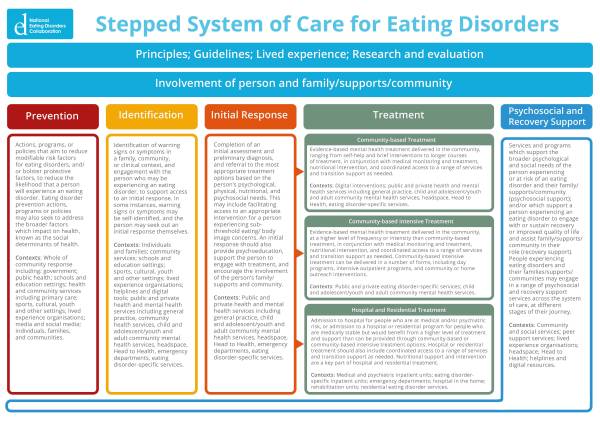
Click here to view.
Click here to see an interactive version.
Click on the drop down boxes to read more about each of the different levels.
Prevention
Eating disorder prevention refers to actions, programs, or policies that aim to reduce modifiable risk factors for eating disorders, and/or bolster protective factors, to reduce the likelihood that a person will experience an eating disorder. Eating disorder prevention actions, programs or policies may also seek to address the broader factors which impact on health, known as the social determinants of health.
The whole community has a role in eating disorders prevention, including (but not limited to) government, public health, schools and education settings, and health and community services.
Identification
Identification refers to the detection of warning signs or symptoms, and engagement with the person who may be experiencing an eating disorder, to support access to an initial response. In some instances, warning signs or symptoms may be self-identified, and the person may seek out an initial response themselves.
Identification can occur in a range of contexts, including (but not limited to) families, community services, sports settings, schools and education settings, helplines, health and mental health services including general practice, headspace, Head to Health, Aboriginal Community Controlled Health Services, emergency departments, and eating disorder-specific services.
Initial response
An initial response comprises an initial assessment and preliminary diagnosis, and referral to the most appropriate treatment options based on the person’s psychological, physical, nutritional, and psychosocial needs. This may include facilitating access to an appropriate intervention for a person experiencing sub-threshold eating/body image concerns. An initial response should also provide psychoeducation, support the person to engage with treatment, and encourage the involvement of the person’s family/supports and community.
The initial response may occur in public or private health and mental health services including general practice, child and adolescent/youth and adult community mental health services, headspace, Head to Health, Aboriginal Community Controlled Health Services, emergency departments, and eating disorder-specific services.
Treatment
Treatment extends across three levels of the stepped system of care, with the treatment intensity increasing across these three levels. A person may commence treatment at any level, depending on their needs.
The first treatment level is community-based treatment, which refers to evidence-based mental health treatment delivered in the community, ranging from self-help and brief interventions to longer courses of treatment, in conjunction with medical monitoring and treatment, nutritional intervention, and coordinated access to a range of services and transition support as needed.
Community-based treatment can be delivered through digital interventions and public and private health and mental health services including general practice, child and adolescent/youth and adult community mental health services, headspace, Head to Health, Aboriginal Community Controlled Health Services, and eating disorder-specific services.
The second level of treatment is community-based intensive treatment, which refers to evidence-based mental health treatment delivered in the community, at a higher level of frequency or intensity than community-based treatment, in conjunction with medical monitoring and treatment, nutritional intervention, and coordinated access to a range of services and transition support as needed. Community-based intensive treatment can be delivered in a number of forms, including day programs, intensive outpatient programs, and community or home outreach interventions.
Community-based intensive treatment can be delivered through public and private eating disorder- specific services and child and adolescent/youth and adult community mental health services.
The third treatment level is hospital and residential treatment, which refers to admission to hospital for people who are at medical and/or psychiatric risk, or admission to a hospital or residential program for people who are medically stable but would benefit from a higher level of treatment and support than can be provided through community-based or community-based intensive treatment options. Hospital or residential treatment should also include coordinated access to a range of services and transition support as needed. Nutritional support and intervention are a key part of hospital and residential treatment.
Hospital treatment can be delivered through medical and psychiatric inpatient units, eating disorder-specific inpatient units, emergency departments, hospital in the home, and rehabilitation units. Residential treatment is delivered through residential eating disorder services.
Psychosocial and recovery support
Psychosocial support refers to services and programs which support the broader psychological and social needs of the person experiencing or at risk of an eating disorder and their family/supports and community. Recovery support refers to services and programs which support a person experiencing an eating disorder to engage with or sustain recovery or improved quality of life and assist family/supports and community in their caring role. People experiencing eating disorders and their families/supports and communities may engage in a range of psychosocial and recovery support services and programs across the system of care, at different stages of their journey.
Psychosocial and recovery support can be delivered through community and social services, health and mental health services including primary care, headspace, and Head to Health, lived experience organisations, peer support services, and helplines and digital resources.
Introduction to the Stepped System of Care eLearning
Introduction to the Stepped System of Care is a brief eLearning outlines the stepped system of care for eating disorders in an interactive way, to support your understanding.

