Anorexia nervosa
Any person, at any stage of their life, can experience an eating disorder. More than one million Australians are currently living with an eating disorder (1).
Of people with eating disorders, 3% have anorexia nervosa compared to 12% with bulimia nervosa, 47% with binge eating disorder and 38% with other eating disorders (1). Of people with anorexia nervosa, 80% are female (2).
Eating disorders are not a choice but are serious mental illnesses. Eating disorders can have significant impacts on all aspects of a person’s life – physical, emotional and social. The earlier an eating disorder is identified, and a person can access treatment, the greater the opportunity for recovery or improved quality of life.
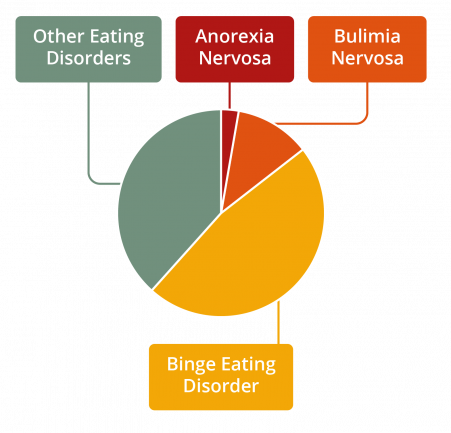
Figure 1. Prevalence of eating disorders by diagnosis
What is anorexia nervosa?
A person with anorexia nervosa will experience significant weight loss due to food restriction and starvation together with an intense fear of gaining weight.
Anorexia nervosa is a serious, potentially life-threatening mental illness. Anorexia nervosa is characterised by restriction of energy intake leading to significantly low body weight accompanied by an intense fear of weight gain and body image disturbance. Changes that happen in the brain because of starvation and malnutrition can make it hard for a person with anorexia nervosa to recognise that they are unwell, or to understand the potential impacts of the illness.
Atypical anorexia nervosa is a subtype of other specified feeding or eating disorders (OSFED). A person with atypical anorexia nervosa will meet all of the criteria for anorexia nervosa, however, despite significant weight loss, the person’s weight is within or above the normal BMI range. Atypical anorexia nervosa is serious and potentially life-threatening, and will have similar impacts and complications to anorexia nervosa.
Subtypes of anorexia nervosa
Restricting type
A person with the restricting subtype of anorexia nervosa severely restricts energy intake and weight loss occurs primarily through dieting, fasting and/or excessive exercise. Recurrent episodes of binge eating or purging behaviour have not been observed in the past three months.
Binge-eating/purging type
A person with this subtype of anorexia nervosa severely restricts energy intake and has also engaged in recurrent episodes of binge eating or purging behaviour (e.g. self-induced vomiting, misuse of laxatives) during the past three months.
Characteristics of anorexia nervosa
Restriction of energy intake
A person with anorexia nervosa will be restricting their energy intake below the amount their body needs to function, leading to significantly low body weight. In children, this is a weight that is below what is minimally expected for them.
Fear of gaining weight
A person with anorexia nervosa has an intense fear of gaining weight, or persistent behaviour that interferes with weight gain, despite being of a low body weight.
Body image disturbance
A person with anorexia nervosa experiences a disturbance in the way in which their body weight or shape is experienced, significant influence of body weight or shape on self-evaluation, and/or persistent lack of recognition of the seriousness of their low body weight.
Risk factors
The elements that contribute to the development of anorexia nervosa are complex, and involve a range of biological, psychological, and sociocultural factors. Any person, at any stage of their life, is at risk of developing an eating disorder. An eating disorder is a mental illness, not a choice that
someone has made.
Warning signs
The warning signs of anorexia nervosa can be physical, psychological, and behavioural. It is possible for a person with anorexia nervosa to display a combination of these symptoms, or no obvious symptoms.
Physical
• Sudden weight loss, frequent weight changes, persistent low weight
• Inability to maintain normal body weight for age and height, failure to grow as expected
• Loss or disturbance of menstruation
• Fainting or dizziness
• Sensitivity to the cold
• Bloating, constipation, or the development of food intolerances
• Fatigue or lethargy
• Fine hair appearing on face and body
• Loss or thinning of hair
• Signs of vomiting such as swollen cheeks or jawline, calluses on knuckles or damaged teeth
• Stress fractures, bone pain, muscle cramps
• Compromised immune system (e.g., getting sick more often)
• Sleep disturbances
Behavioural
• Repetitive dieting behaviour such as counting calories, skipping meals, fasting or avoidance of certain foods or food groups
• Evidence of vomiting or misuse of laxatives, appetite suppressants, enemas and/or diuretics
• Frequent trips to the bathroom during or shortly after meals
• Patterns or obsessive rituals around food, food preparation and eating
• Change in food preferences
• Avoidance of, or change in behaviour in social situations involving food
• Social withdrawal or isolation from friends and family
• Secretive behaviour around eating
• Patterns or obsessive behaviours relating to body shape and weight
• Compulsive or excessive exercising
• Substance misuse
• Continual denial of hunger
• Drinking too much or too little
• Change in clothing such as wearing baggy clothes or more layers than appropriate for the weather
Psychological
• Preoccupation with eating, food, body shape or weight
• Intense fear of gaining weight
• Preoccupation with food or activities relating to food
• Heightened anxiety or irritability around mealtimes
• Heightened sensitivity to comments or criticism (real or perceived) about body shape or weight, eating or exercise habits
• Low self-esteem and feelings of shame, self-loathing or guilt
• Body dissatisfaction or negative body image
• Difficulty concentrating
• Obsession with food and need for control
• ‘Black and white’ thinking - rigid thoughts about food being ‘good’ or ‘bad
It is never advised to ‘watch and wait’. If you or someone you know may be experiencing an eating disorder, accessing support and treatment is important. Early intervention is key to improved health and quality of life outcomes.
Impacts and complications
A person with anorexia nervosa may experience serious medical and psychological consequences. (3, 4) Some of the impacts and complications associated with anorexia nervosa include:
Medical
• Anaemia
• Osteoporosis or osteopenia: a reduction in bone density caused by a specific nutritional deficiency
• Heart problems including slow heart rate, irregular heartbeat and low blood pressure
• Electrolyte disturbance, including potassium and sodium
• Malnutrition
• Fatigue and lethargy
• Loss of or disturbance to menstruation
• Impairment of kidney, liver, or pancreatic function
• Gastrointestinal problems
• Increased risk of infertility
• Delayed growth
• Death
Psychological
• Extreme body dissatisfaction/distorted body image
• Obsessive thoughts and preoccupation with eating, food, body shape and weight
• Social withdrawal
• Feelings of shame, guilt, and self-loathing
• Depressive or anxious symptoms and behaviours
• Self-harm or suicidality
• Substance misuse
Treatment options
Access to evidence-based treatment has been shown to reduce the severity, duration and impact of anorexia nervosa.
Evidence-based psychological therapies to consider for the treatment of anorexia nervosa in children and adolescents include:
- Family-based treatment (FBT) or family therapy for anorexia nervosa (parent-focused and multi-family group also acceptable)
- Eating disorder-focused CBT (CBT-ED) enhanced with family involvement
- Adolescent-focused psychotherapy (5)
Evidence-based psychological therapies to consider for the treatment of anorexia nervosa in adults include:
- Maudsley anorexia nervosa treatment for adults (MANTRA)
- Specialist supportive clinical management (SSCM)
- Eating disorder-focused CBT (CBT-ED)
- Eating disorder-focused focal psychodynamic therapy (5)
Most people can recover from an eating disorder with community-based treatment. In the community, the minimum treatment team includes a medical practitioner such as a GP and a mental health professional.
Inpatient treatment may be required when a person needs medical and/or psychiatric stabilisation, nutritional rehabilitation and/or more intensive treatment and support.
Recovery
It is possible to recover from anorexia nervosa, even if a person has been living with the illness for many years. The path to recovery can be long and challenging, however, with the right team and support, recovery is possible. Some people may find that recovery brings new understanding, insights and skills.
Getting help
If you think that you or someone you know may have anorexia nervosa, it is important to seek help immediately. The earlier you seek help the closer you are to recovery. Your GP is a good ‘first base’ to seek support and access eating disorder treatment.
To find help in your local area go to NEDC Support and Services.
Download the anorexia nervosa fact sheet here.
References
1. Deloitte Access Economics. Paying the price: the economic and social impact of eating disorders in Australia. Australia: Deloitte Access Economics; 2012.
2. Hay P, Girosi F, Mond J. Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian population. J Eat Disord. 2015;3(1):1-7.
3. Gibson D, Workman C, Mehler PS. Medical complications of anorexia nervosa and bulimia nervosa. Psychiatr Clin North Am. 2019;42(2):263-74.
4. Allen KL, Byrne SM, Oddy WH, Crosby RD. DSM–IV–TR and DSM-5 eating disorders in adolescents: prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. J Abnorm Psychol. 2013;122:720-32.
5. Heruc G, Hurst K, Casey A, Fleming K, Freeman J, Fursland A, et al. ANZAED eating disorder treatment principles and general clinical practice and training standards. J Eat Disord. 2020;8(1):63.

