Issue 77: Turning Research into Reality
About this resource
New NEDC resources rolled out plus updated Medicare and Treatment info
Interview with Dr Andrea Phillipou, head of Swinburne Anorexia Nervosa (SWAN) Research Group
Interview with Jodie Ashworth, Executive Director and Director of Nursing Wandi Nerida
NEDC launches Eating Disorders Quality Improvement Tool for Primary Health Networks
Body Image & Related Disorders (BIRD) Conference report
Editor’s Note
This edition of the NEDC eBulletin showcases how people and organisations are using the latest research and up-to-date knowledge and evidence to create a better system of care for people with eating disorders.
Turning research studies into improved clinical practice and better outcomes for people experiencing eating disorders is practical, effective, and important work. It can take several years from identification to implementation and involves different people at different stages of development. Planning, consultation, testing, publishing, piloting, and implementation all have a role to play along the way.
For NEDC, this includes updating our fact sheets and resources for GPs, other health professionals and for people with lived experience to reflect the latest research and best practice; developing and launching the interactive Eating Disorders Quality Improvement Tool for PHNs (ED QI); consulting on and developing the clinical guidelines for the management of eating disorders for people with higher weight; and reporting on international research presented at the recent BIRD Conference. In two interviews with leaders in the field, in this issue we delve into SWAN’s ground-breaking discoveries in eye movement and implications for treatment for people experiencing anorexia nervosa, and Australia’s first purpose-built residential treatment facility for people with eating disorders, Wandi Nerida.
You can read about NEDC’s updated resources here and access resources here, including booklets:
fact sheets:
- Eating Disorders and Diabetes
- Eating Disorders in Males
- Medicare Items for Eating Disorders – Cheat sheet for GPs
an infographic:
and updated website pages:
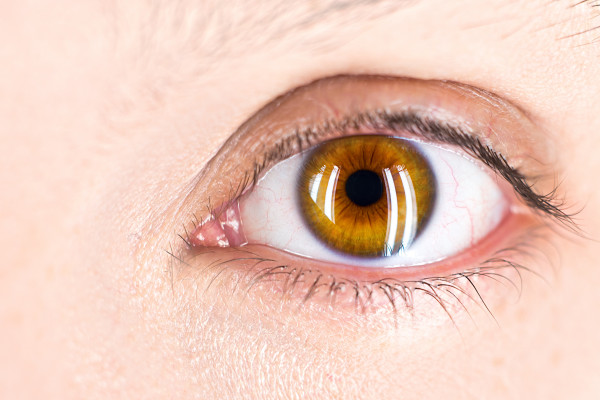
In October, Swinburne Anorexia Nervosa (SWAN) Research Group released a ground-breaking study suggesting that atypical eye movement, called square wave jerks, together with anxiety, may represent a biomarker and endophenotype for anorexia nervosa. We spoke to SWAN’s Dr Andrea Phillipou about this research, the COVID-19 COLLATE Project and the importance of lived experience involvement in research. “Eye movements are really cool because they can tell us so much,” she said. Read our interview here.
Jodie Ashworth, Wandi Nerida Executive Director and Director of Nursing, spoke to us about opening Australia's first purpose-built residential treatment facility for people with eating disorders during COVID-19. "Wandi Nerida fills the gap between acute hospital admissions and community care by offering residential treatment for participants to focus on psychological recovery while (being) supported medically," she said. Read our Q&A here.
Eating disorders should be “viewed as core business within the primary mental health care system”, said the Hon David Coleman MP, Assistant Minister to the Prime Minister for Mental Health and Suicide Prevention, at the launch of NEDC’s Eating Disorders Quality Improvement Tool for PHNs (ED QI). Find out how this innovative, purpose-built tool can help PHNs support better outcomes for Australians experiencing or at risk of developing an eating disorder here.
Bringing together academic, clinical, and lived experience expertise, over 2020-2021 NEDC have led the development of clinical practice guidelines for the management of eating disorders in people with higher weight. As part of the review process, we are now seeking public feedback and invite our members to be involved in this consultation. Find out how you can have your say here.
NEDC’s National Manager Dr Sarah Trobe and NEDC Workforce Development Coordinator Dr Emma Spiel attended the virtual Body Image and Related Disorders (BIRD) Conference. Read their report on the latest local and international research into body image, anorexia nervosa and body dysmorphic disorder here.
NEDC rolls out more updated resources
Aligned with the DSM-5, fully referenced, and downloadable in PDF, our latest updated resources are useful for people with lived experience, families and supports to better understand eating disorders, and for clinicians and health practitioners to increase literacy and awareness of eating disorders in their clients and patients.
The most up-to-date data and statistics have informed our new booklet Eating Disorders in Australia. Who is affected and how are they affected? Readers can find facts quickly with a breakdown of eating disorder types, prevalence in the general population and according to age and gender, warning signs, impacts, medical and psychological complications, mental health and medical comorbidities, types of treatment, recovery and getting help.
The prevalence of males experiencing an eating disorder may be much higher than the data indicates. This under-reporting may be related to underdiagnosis, misdiagnosis, and the stigma associated with eating disorders in males. Just in time for Movember, we have updated our fact sheet Eating Disorders in Males and infographic Males experience eating disorders too with the latest information on prevalence, the development of eating disorders in males, the physical, psychological and behavioural warning signs, body dysmorphic disorder, recovery, treatment options and getting help.
Eating disorders are more common in people with type 1 diabetes when compared to their peers without type 1 diabetes. For people with type 2 diabetes, it is estimated that 12% to 40% have an eating disorder On World Diabetes Day, 14 November, we launched our newest fact sheet Eating Disorders and Diabetes, which outlines the complex links between eating disorders and type 1 and type 2 diabetes, ‘diabulimia’, risk factors and potential triggers, warning signs, health consequences and treatment.
The role of the GP is crucial in supporting people experiencing an eating disorder. But what does this role involve? NEDC’s booklet Eating Disorders: A professional resource for general practitioners has been updated to align with NEDC’s comprehensive foundational online eating disorder training, Eating Disorder Core Skills: eLearning for GPs. Here, GPs can find a guide to screening, assessment, the treatment team, medical monitoring and more. There is also a handy Medicare Items for Eating Disorders – Cheat sheet for GPs which has tips on assessment, developing an Eating Disorders Treatment and Management Plan (EDP), relevant MBS item numbers and a useful flowchart outlining the pathway a person experiencing an eating disorder takes to access treatment.
New Medicare items were introduced for people experiencing anorexia nervosa and other eating disorders in 2019. But who is eligible? How can a medical practitioner complete an EDP and who else is involved? It can be confusing navigating the supports available under the MBS, including Eating Disorder Treatment and Management Plans (EDP), Mental Health Treatment Plans (MHTP) or Chronic Disease Management (CDM) Plans. Our Eating Disorder Medicare Items page has been updated to help professionals, people with lived experience, families and supports find their way to accessing treatment. Read our guide to Eating Disorder Medicare Items here, and we also take you step-by-step through the treatment pathway of an EDP, including approved psychological treatments, reviews and referrals on our Eating Disorder Treatment and Management Plans page here.
Dr Andrea Phillipou interview
Dr Andrea Phillipou is a Senior Research Fellow, and Head of the Swinburne Anorexia Nervosa (SWAN) Research Group and the Body Image & Eating Disorders Research Portfolio at St Vincent’s Hospital in Melbourne. She spoke with us about her research into biopsychosocial factors and into development of anorexia nervosa, the COLLATE COVID-19 project and the importance of lived experience.
Tell us about how you became involved in the eating disorders sector and your particular field of interest.
My aunty had anorexia nervosa for as long as I can remember and died from the illness at the age of 35. She was one of those few special people you meet in your life who everyone loves and adores, and I couldn’t understand why and how her entire life became totally consumed, and ultimately taken, by this illness. She had been in and out of treatment for most of her adult life, but nothing worked. She hadn’t failed treatment, but the treatments available at the time had failed her. It’s been 13 years since she lost her life, and sadly, we haven’t made much progress in improving treatment outcomes since then.
My research is therefore centred on improving the lives of people with anorexia nervosa – specifically, how we can improve prevention, early identification and treatment. A key focus of the work I do is to investigate the underlying factors involved in causing anorexia nervosa. To me, it’s always seemed logical that if we want to effectively prevent or treat any illness, we first need to know what leads to its development and maintenance; otherwise, what are we treating?
Last month you released ground-breaking research A biomarker and endophenotype for anorexia nervosa? (Phillipou et al., 2021) This study suggested that atypical eye movement, called square wave jerks, together with anxiety, may represent a biomarker and endophenotype for anorexia nervosa. Your interest in in eye movement assessments and eyetracking has been longstanding, spanning a 2014 paper, Square wave jerks and anxiety as distinctive biomarkers for anorexia nervosa (Phillipou, 2014), and more recently Eye movements in anorexia nervosa: State or trait markers? (Phillipou et al., 2020) and Current directions in biomarkers and endophenotypes for anorexia nervosa: A scoping review (Malcolm & Phillipou, 2021). What are the implications of this research? What is the next step with this research?
Eye movements are really cool because they can tell us so much, non-invasively. We have a really good understanding of the brain circuits involved in how we move our eyes, so when the eyes don’t move like we’d expect them to, it can tell us about very specific brain regions that aren’t functioning correctly. And like all parts of the brain, these regions don’t have just one function, but are involved in multiple different processes that are relevant to mental illness.
So our research in this area really started out with this aim of getting a better understanding of the neurobiological contributions to anorexia nervosa, so we could develop treatments that specifically target the underlying neurobiology of the illness. We, however, didn’t expect there to be such distinct eye movement differences in people with anorexia nervosa, and that we’d able to use this to accurately identify people with the illness, from those without, with such high accuracy. With more research, we’re hoping we can use this biomarker for both early intervention as well as prevention.
In terms of next steps, we have a couple of projects in the works. The first is a large-scale study that aims to test over 300 people to establish the utility of this biomarker for anorexia nervosa; and we were very fortunate to receive NHMRC project funding to do this work. The second study is a pilot investigation using non-invasive brain stimulation to target the brain regions that have been implicated, in the hope that it will improve symptoms. We’re excited to kick off both of these studies again once the COVID situation in Melbourne has resolved.
Swinburne Anorexia Nervosa (SWAN) Research Group conducted the COLLATE project since the beginning of the COVID-19 pandemic. These anonymous online surveys provided a monthly snapshot of Australians’ experiences during this time. COLLATE studies include perceptions about eating and exercise behaviours, mask use, alcohol use, OCD symptoms, mental health status of healthcare versus other essential workers and even pet ownership. Mental health of individuals with and without eating disorders across six months and two waves of COVID-19 (Phillipou et al., 2021) concluded that “Although non-ED and ED groups tended to generally show the same pattern of symptoms, the mental health status of the ED group was significantly poorer than the non-ED group throughout the pandemic, and exacerbations in some symptoms (i.e. increased food restriction and depressive symptoms) is cause for concern.” What else have you learned from this project about how people with lived experience of eating disorders have coped with the pandemic?
The COLLATE project is a collaborative study run through the Centre for Mental Health at Swinburne, and led by Prof Susan Rossell. We’ve learned so much about the mental health impacts of the COVID-19 pandemic on people in Australia, and people with eating disorders, specifically. The pandemic has been very difficult for people with eating disorders, particularly people living in areas who have experienced multiple and prolonged lockdowns, such as in Melbourne. During lockdowns in particular, we’ve seen increased eating disorder behaviours and poorer mental health in both people with and without eating disorders. Although we’re seeing similar patterns across time, people with eating disorders have started off with more severe symptoms which are being exacerbated throughout the pandemic. The long-term impacts of the pandemic on mental health are likely to continue for some time, but the somewhat promising news is that symptoms seem to improve when we start emerging from lockdown.
You contributed to Valuing the voice of lived experience of eating disorders in the research process: Benefits and considerations (Music et al., 2021), which was presented as a workshop at the recent ANZAED Conference. How important is lived experience to your work?
The voice of lived experience is central to the research we do in our group, and should be central to all research in eating disorders. People with lived experience bring so much knowledge, and are truly experts by experience. We actively collaborate with people with lived experience on research and their input has been invaluable – from helping to identify meaningful research that we should be undertaking, to giving their unique insight into the interpretation of research findings. We’re so grateful to have the contribution of people with lived experience guide the work that we do, and to be able to work with them in such a close and collaborative way.
In A biopsychosocial proposal to progress the field of anorexia nervosa (Phillipou et al., 2019), you note that in stark contrast to many other mental illnesses, with anorexia nervosa “we have arguably made little progress in uncovering the aetiological and maintenance factors involved in the illness, and in developing effective treatments”. Do you think a biological approach might be more successful?
Like all mental illnesses, biological, psychological and sociocultural factors are likely to contribute to the development of anorexia nervosa, so they’re all important to understand. For some people, psychological or sociocultural factors may have played a bigger role, while for others, biological factors may have been the stronger driving force. For most people, it’s likely a combination of different biopsychosocial factors. While our research is interested in looking at factors across the biopsychosocial spectrum, we have a particular focus on the biological mechanisms. We have a relatively good understanding of some of the psychological and sociocultural factors that can contribute to anorexia nervosa, but everyone who’s exposed to these things doesn’t go on to develop anorexia nervosa; which suggests there’s likely an underlying biological or neurobiological predisposition to developing the illness that we need to better understand so that we are able to treat the illness better.
As the lead of the Swinburne Anorexia Nervosa (SWAN) Research Group, and the Body Image & Eating Disorders Research Portfolio at St Vincent's Hospital, can you tell us what you hope attendees can learn from the Body Image and Related Disorders (BIRD) Conference?
We started running the BIRD Conference in 2017 with the aim of bringing together researchers, clinicians, people with lived experience, those working in the not-for-profit sector, and anyone else with an interest in body image and eating disorders. The conference is focused on presenting some of the most exciting developments in eating disorders research in a way that’s not too ‘research-y’ or focused solely on clinicians. It’s an opportunity for anyone who’s interested in learning more about new findings in eating disorders research to do so. In order to ensure as many people who’d like to attend the conference are able to, we ensure registration fees are as low as possible to cover the costs of the conference. This year, we’re excited to have been able to hold a virtual conference without any cost, welcoming almost 1000 people from all around the world. (For NEDC’s report on the BIRD conference, click here.)
In 2022, you will be guest editor of the Journal of Clinical Medicine, publishing a Special Issue in 2022 titled "Advances in the Aetiology and Treatment of Anorexia Nervosa". Submissions are open until 15 March. What contributions are you interested in receiving?
We’d love to receive submissions on any aspect of factors that might contribute to the development of anorexia nervosa, as well as findings of any treatment studies. The special issue will also include review papers, so submissions on any aspect of the aetiology or treatment of anorexia nervosa are also very welcome.

Dr Andrea Phillipou is a Senior Research Fellow, and Head of the Swinburne Anorexia Nervosa (SWAN) Research Group and the Body Image & Eating Disorders Research Portfolio at St Vincent’s Hospital. Andrea’s research is focused on using neuro-bio-psycho-social methods to gain a better understanding of the factors involved in anorexia nervosa, to develop tools for early intervention and prevention, and to develop more effective treatments.
Jodie Ashworth interview
Jodie Ashworth, Wandi Nerida Executive Director and Director of Nursing, leads the team at Australia's first purpose-built residential treatment facility for people with eating disorders. She tells us about the centre's model of care, programs and services and her hands-on role, which includes supporting equine-assisted therapy, meal therapy and even snake removal.
How did you become involved in the eating disorder sector? What changes have you seen and what would you like to see?
I first became involved in the eating disorder sector when my daughter was suffering from bulimia. She was in year nine (when) the Butterfly Foundation came and did a presentation at her school in country Victoria. I remember her coming home and telling me about it. She was 14 and it was the first time we really discussed the topic openly. Our family had its own journey for a while there and much later, when we moved to Queensland, I became aware of the Wandi Nerida vision through Anne Doherty, a member of the BF [Butterfly Foundation] Board. My daughter, now fully recovered, encouraged me to be involved. It was time to give back and do some purposeful work.
The biggest changes I have seen are the busting of some of the myths around eating disorders, particularly that you need to be very under or overweight to have an ED and that they only affect a certain gender, race or class of people. What I would like to see more of is a breakdown and cessation of our diet culture and the acceptance of different body sizes as the norm, particularly in adolescents. I would also love to build on the research for the treatment for eating disorders. Wandi Nerida and the B-FREEDT model of care is part of a clinical and economic evaluation over several years and I’m looking forward to understanding these outcomes.
Wandi Nerida is Australia’s first purpose-built residential treatment facility for people with eating disorders. Can you tell us about your role at Wandi Nerida?
Lol, I am a very lucky person - my role can look different every day of the week! I am the Executive Director at Wandi Nerida, so one of my main jobs is to lead the executive team to set the strategies that ensure we deliver on the B-FREEDT model of care, ensure we deliver a safe and quality service and always ensure our care is participant centred.
As I am also the Director of Nursing, it is not uncommon for me to have a clinical role as well. For example, I am involved in equine assisted therapy at Wandi Nerida, (and) often do supported meal therapy and other clinical roles. This week I need to organise for the carpet python snake to be removed from our chicken coop despite that not being in my PD!
The name Wandi Nerida is a term gifted by local Elders of the Kabi Kabi nation meaning to ‘gather together to blossom’. What is Wandi Nerida’s role in eating disorder treatment in Australia?
Wandi Nerida fills the gap between acute hospital admissions and community care by offering residential treatment for participants to focus on psychological recovery while (being) supported medically. In many ways it is the “step up/step down” facility for eating disorder recovery. For example, many participants step down to us from tertiary hospital care once they are medically stable but need a little more support and time for psychological recovery. It is the opposite for community care - we offer a step up to the next level of support for participants who need a little more support than can be received in a community setting. There is a definite focus on the residential model. We have tried to promote a home-like environment and build a social milieu that concentrates on connection with staff and other participants.
Can you tell us about the Wandi Nerida model of care? What are some of the programs and services offered?
Wandi Nerida utilised the B-FREEDT model of care which Butterfly Foundation has developed for the Australian residential context. It aims to support individuals to help make recovery from an eating disorder a reality. The model of care includes a phase-based system to support participants to challenge their eating disorder with increasing levels of independence. The program is founded in Carolyn Costin’s principles, and the philosophy outlined in her book 8 Keys to Recovery from an eating disorder.
The clinical program includes evidence-based treatment groups such as CBT, DBT, individual therapy, mindfulness group and nutrition groups. In addition, we incorporate the use of complementary therapies such as the equine program, nature-based therapy, yoga, and art/drama. Wandi Nerida believes in the power of lived experience in the recovery journey and provides lived experience support within the staff team and through support groups. The program is intensive with a timetable that operates from 8am -8pm 7 days a week.
Who is Wandi Nerida designed to help? Is the facility mainly for people with an eating disorder who are struggling with repeated hospitalisations and relapses in recovery?
Wandi Nerida is designed to be a step in the continuum of care for people with eating disorders. This can act as a different intervention for people who are struggling with repeated admissions. Alternatively, it can provide a higher level of support for individuals who have found that community-based treatment does not meet their needs who may have never had a hospital admission. Wandi Nerida provides treatment for individuals with a range of eating disorders including bulimia nervosa, anorexia nervosa and binge eating disorder, many of whom may not have had hospitalisations. Wandi Nerida hopes to provide a supportive residential treatment model for all individuals wanting to work towards their recovery.
By launch day in June, Wandi Nerida had received more than 660 enquiries from people looking for potential admission for themselves or a loved one. How can people register their interest?
We have a referral process that can be accessed through wandinerida.hothealth.com. There is information on this site for both clinicians and future participants. In addition, we have a web page wandinerida.org.au which has further information on it.
Due to COVID-19, there has been increased demand for eating disorder support with lockdowns causing disruptions to services. How can Wandi Nerida help?
Wandi Nerida has been fully operational throughout the Covid period and we have continued to support participants and families throughout this time. It’s been really difficult for some of our participants from interstate as families have not been able to get across the border to visit them and quarantine requirements have been challenging. We have had to make several changes to our timetable to accommodate Covid requirements but have continued to operate at full capacity as we know the demand is high.
NOTE for health professionals: Wandi Nerida centre usually has a waiting list, but due to Queensland border restrictions and COVID disruptions in other states some beds are available. With Queensland quarantine orders likely to be lifted by December 17, this is a rare opportunity for eating disorder professionals to refer their clients, particularly those in Queensland, WA, SA and NT who are able to enrol at short notice.
To find out more or to refer a client, click here.

Jodie Ashworth has more than 30 years of experience in the Australian public health sector as a registered nurse, midwife, quality director, and executive leader of large public health services. During her career she has worked across three states and territories of Australia in remote, regional and metropolitan health services. She is a leader with a proven track record in service development, quality improvement and risk management. Before her appointment as Wandi Nerida Chief Executive, Jodie’s most recent role was as the Acting Executive Director of Operations for the Metro North Hospital and Health Services. Jodie holds a Diploma in Applied Science Nursing and Post Graduate Diplomas in Health Service Management, Midwifery, Critical Care and Human Resources. She is also a current Accredited Surveyor for National Standards, Equip National & Community Services. Jodie has led the team at Wandi Nerida to open the facility in July 2021, despite the many challenges that COVID has brought. This includes finalising the model of care, staff recruitment and training along with ensuring Wandi Nerida meets the QLD standards for a private licenced facility. She has also led the team to achieve interim accreditation under the National Safety and Quality Health Service (NSQHS) Standards which enables the participants to be able to access private health insurance. Wandi Nerida welcomed its first 13 participants in July of 2021.
PHN ED-QI tool launch
NEDC launched the Eating Disorders Quality Improvement Tool for PHNs (ED QI) on Wednesday, 10 November. The ED QI is an innovative, engaging new purpose-built tool developed alongside Primary Health Network (PHN) leaders, people with a lived experience, and eating disorder experts.
The ED QI guides PHNs through the process of building on their eating disorders response. There are 20 best practice actions focused on strategies in Operational Resources and Planning, Awareness Raising and Information Provision, Primary Care Improvement and Service Integration and Coordination. The tool begins with online self-assessment, which generates a downloadable personalised service plan and action planning worksheet to assist PHNS to plan the next steps to implementing best practice actions.
The launch featured the Hon David Coleman MP, Assistant Minister to the Prime Minister for Mental Health and Suicide Prevention, who affirmed the significance of this work and the role that PHNs play in supporting better outcomes for Australians experiencing or are at risk of developing an eating disorder.
Click here to watch the video.
National Director Dr Beth Shelton shared the story of how NEDC has developed the ED QI, always working with the aim “to deliver something actually useful”. Since 2018, NEDC has worked collaboratively with PHNs to develop the tool, including piloting the draft ED QI with seven PHNs and incorporating feedback to deliver an online and interactive tool that is aligned with PHN work areas and is “well-matched to the PHN context and delivers achievable next steps”. Dr Shelton reiterated that “PHN lean-in and engagement will significantly change things for the better with Australians experiencing eating disorders”.
The launch webinar featured a demonstration of the ED QI and the NEDC were joined in an informative Q&A by panellists Paul Martin, Executive Manager, Mental Health, Alcohol and Other Drugs at Brisbane North PHN, and Lauren Hendriks, Director, Adult Mental Health Services, at the Australian Government Department of Health.
How do PHNs prioritise this work among competing demands, especially among the ongoing response to COVID-19? Paul Martin reflected that the ED QI is a tool that provides everything all in one place, written specifically for PHNs, about making the things PHNs already do easier and more informed; and that it has been developed by experts and people with a lived experience. Paul emphasized that the ED QI makes the work easier.
The ED QI is a user-friendly, practical tool, that will support PHNs to plan and implement best practice solutions, to respond to eating disorders in their regions. To find out more, click here.
The ED QI preview can also be viewed here.
Watch the launch recording here.

Bronwyn Scott is NEDC’s Primary Health Lead working with Australia’s Primary Health Networks to support their response to eating disorders. She has a lived experience of an eating disorder and knows firsthand the benefit of a multidisciplinary and coordinated approach to care. Her work builds strong and collaborative relationships that have multi-layered impact in the health system. As an accredited practising dietitian, her focus has been on the structures that support access to appropriate, affordable, and timely care particularly in issues relating to nutrition and health. Her clinical experience has included work in private practice, and in intensive outpatient programs for youth and adults experiencing eating disorders.
Have your say about new guidelines
The National Eating Disorder Collaboration (NEDC) Steering Committee has convened a Guideline Development Group to create, write and develop the ‘Management of eating disorders for people with higher weight: clinical practice guidelines’. The Guideline Development Group includes academic, clinical, and lived experience expertise.
The aim of the guideline is to synthesise the current best practice approaches to the management of eating disorders in people who are at higher weight. This is based on the premise that every person with an eating disorder is deserving of equitable, safe, accessible, and evidence-based care regardless of their body size. It accords with the role and function of NEDC to synthesise research evidence, clinical expertise, and lived experience in national standards to improve systems of care for all Australians experiencing an eating disorder.
Throughout 2021, this guideline has undergone extensive review and consultation with key stakeholders including experts and organisations with clinical, academic and/or lived experience. NEDC and the Guideline Development Group are now seeking public feedback on the guideline, and we invite you to be involved in this consultation.
The public consultation will begin 18 November until 2 December.
To access the document please click here.
To access the online form to submit feedback, please click here.
or scan the QR code 

Dr Angelique Ralph is NEDC's Research Lead. She completed her PhD at the School of Psychology at the University of Sydney and has held research positions at the Sydney School of Public Health at the University of Sydney and in the School of Women and Children’s Health at the University of New South Wales. She is passionate about research translation, that is, bridging the gap between knowledge and action through making high-quality research accessible and relevant to those who can use it. Angelique is also a clinical psychologist and has held clinical positions at the Peter Beumont Eating Disorder Service and Children’s Hospital at Westmead. She currently works with people living with eating disorders in private practice and has a particular interest in working with adults with severe and enduring eating disorders, people with higher weight and people with comorbid chronic conditions.
BIRD Conference report
The Swinburne Anorexia Nervosa (SWAN) Research Group hosted the 3rd biennial Body Image and Related Disorders (BIRD) conference on Friday 12 November. The virtual conference brought together leading local and international experts in the field of body image and eating disorders with sessions broadly covering research in anorexia nervosa, body image, lived experience involvement in body image and related disorders research, and body dysmorphic disorder.
Professor Joanna Steinglass from Columbia University spoke about translational research in understanding the neurocognitive mechanisms behind restrictive eating in anorexia nervosa and how these findings can guide new treatment approaches. Professor Steinglass and her team have been exploring the role of the dorsal striatum in food choice and food restriction and propose that behavioural approaches designed to interrupt restricting eating behaviour patterns and shifting related cognitions could be an effective treatment approach for people experiencing anorexia nervosa.
Other research from the SWAN team has explored cognitive inflexibility in people experiencing anorexia nervosa as well as the psychophysiology in anorexia nervosa. These findings can help both mental health and medical treatment providers to better understand the cognitive and physical mechanisms and/or outcomes of anorexia and effectively target their interventions.
Research presented on body image and eating disorders showcased leading efforts aimed at leveraging digital technology to reduce eating disorders and highlighted the importance of understanding diversity in eating disorder experience, so that we may better respond to the specific needs of groups such as First Nations Australians, and sexual minority women.
Presentations related to body dysmorphic disorder outlined research which supported better understanding of treatment response, as well as the role of hallucinations, shame and identity in how we better understand and work with people to help them overcome body dysmorphic disorder.
A key theme threaded throughout the conference was the importance of meaningfully incorporating lived experience perspectives across all research activities including the role of lived experience researchers, participants, and engaging in research codesign.
Thank you to the SWAN team for making this information freely accessible to so many people and for your continued work into understanding body image and related disorders.
If you were not able to attend the event, you can email birdconference@swin.edu.au to receive a link to the recorded conference proceedings.
NEDC National Manager Dr Sarah Trobe and NEDC Workforce Development Coordinator Dr Emma Spiel