Issue 76: Online tools and programs
About this resource
Eating Disorders Queensland, Shared Table – Melissa Cheras
CEED, FYI and ROAR – Michelle Roberton
Butterfly Foundation, Body Kind – Helen Bird
Inside Out SupportED – Danielle Maloney
Editor’s Note
At the InsideOut Institute for Eating Disorders they say “it takes a village”. Along with many hands, having access to evidence-based tools and resources is fundamental to enhancing the system of care for the prevention and treatment of eating disorders.
Across Australia, lived experience organisations and service development organisations (see below for definitions of groups involved in the eating disorder sector) have developed free, nationally available online programs aimed at helping people experiencing an eating disorder and their carers access information, skills and knowledge. They have created flexible, evidence-informed resources ranging from interactive checklist and report-generating tools, modular structured courses and skills-based programs encompassing written information, role plays, animations, audio, personal stories and short videos.
With one of the consequences of COVID-19 being an increased demand for eating disorder services, there can be a long waitlist to access health professionals with eating disorder training or longer gaps between appointments. Online programs can help people continue to access supportive resources, increase their health literacy and take steps towards engaging in seeking treatment. Unlike face-to-face, in-person programs, continuously available, self-paced skills-based programs are not limited by geography, transport or time availability.
Many web-based programs also collect valuable data which can help developers understand usage patterns, how people interact with the content, and how the delivery can be improved. Collated and published data can only add to the knowledge base and could inform clinical practice and guidelines in the future.
Created with input from carers, parents, supports, clinicians, body image experts and eating disorder researchers, online programs are a practical and effective addition to the ‘toolbox’ needed to build the system of care.
In 2020 Eating Disorders Queensland launched The Shared Table Supportive Meal Therapy training for carers with two strands: one for families engaged in Family-Based Therapy (FBT) and one for those who are not. The Shared Table is also available for professionals to upskill in providing Supportive Meal Therapy, is self-paced and appropriate for all ages. Read our interview with Eating Disorders Queensland Senior Carer and Family Coach Melissa Cheras here.
The Victorian Centre of Excellence in Eating Disorders (CEED) has two interactive online tools with checklists generating personalised summaries that can be presented to GPs or health professionals: Feed Your Instinct (FYI) is for parents concerned about their child’s relationship with food and their body; and Reach out and Recover (ROAR) is for adults with eating and body image concerns. Read our interview with CEED Manager and Senior Clinician Michelle Roberton here.
The Butterfly Foundation’s latest body awareness initiative is Body Kind Schools and Body Kind Families. This year more than 1,600 schools/organisations registered to Body Kind Schools to receive classroom activities, posters, digital clips and take part in support webinars and educator or peer-led workshops. Body Kind Families features videos, tips-sheets in print and audio format and activities. Read our interview with Butterfly Manager Education Services Helen Bird here.
In 2021 InsideOut Institute for Eating Disorders launched SupportED: Online Self-Help Program for Carers of People with an Eating Disorder. SupportED is a five-module, skills-based program for those who support someone with an eating disorder and provides access to more than 200 resources. It is also the subject of a research study with participants completing questionnaires and providing feedback. Read our interview with InsideOut Deputy Director Danielle Maloney here about SupportED and the Australian Eating Disorder Research and Translation Strategy 2021-2031 and the Top 10 Research and Translation Priorities.
Definitions within the Stepped System of Care:
Service development organisations: organisations that focus on education and training, service improvement and integration, clinical consultation and outreach, and/or policy to guide health services and policymakers to plan for and effectively respond to eating disorders.
Lived experience organisations: organisations which advocate, educate, support, and provide evidence-based information about eating disorders to the broader community (particularly to people with lived experience, including families and supports).
Treatment services: organisations/services that deliver evidence-based treatment for eating disorders, categorised according to the three treatment levels of the stepped system of care for eating disorders.
Peer support work: services or individuals providing non-clinical support to people experiencing an eating disorder, drawing on their own lived experience of an eating disorder (self or carer).
Note: There is some overlap in some groups in activities. For example, some lived experience organisations may also undertake service development activities and/or provide clinical services.
EDQ, The Shared Table - Melissa Cheras
Psychologist Melissa Cheras, Senior Carer and Family Coach at Eating Disorders Queensland, discusses the online program The Shared Table: Meal Support Training for Carers and Professionals. The program provides information, strategies and education for carers and key support people who are supporting a person through eating disorder recovery.
As a psychologist, your previous work has encompassed schools, corrections, private practice and commissioning suicide prevention services. How did you become involved in the eating disorders field?
In my work as a psychologist, I have provided therapeutic support and treatment for adolescents and adults with eating and body image issues. I have always worked from a person-centred and family systems approach and therefore the role at EDQ working within the Carer & Family team very much appealed to me!
Mealtimes can be extremely challenging for families and people living with an eating disorder. Tell us about The Shared Table: Meal Support Training for Carers and Professionals. Is the program open to people outside Queensland? Is there a cost? How is it structured? How interactive is it?
The Shared Table is a free, online meal support training program which was designed specifically to assist carers and key support people in the provision of meal support for their loved one/s. This training can be accessed by carers outside of Queensland. The Shared Table is funded by Metro North Hospital and Health Service LINK Innovation Fund and is a partnership between The Queensland Eating Disorder Service, Eating Disorders Queensland and Child and Youth Mental Health Service Eating Disorders Program (EDP). This online training assists carers and key support people to increase their knowledge and skills and improve their confidence around meal support. The training provides written content along with videos, including with carers with a lived experience of supporting a loved one through eating disorder recovery.
How do you recommend carers and support people use the program? How are concerning behaviours addressed?
Registering for the training allows carers to access the training for as long as required. The modules have been designed for carers to work through at their own pace. The training provides information about the stages of meal support (pre, during and post meal support), communication skills, setting rules, boundaries and non-negotiables, and provides an in-depth look at the role nutrition plays in recovery.
How do you recommend professionals use the program? Is this program used to educate staff providing inpatient meal support?
The Shared Table training was designed for carers and family members providing meal support for their loved one/s. The training is also available for professionals who would like to increase their knowledge, skills and confidence in providing Supportive Meal Therapy.
Adults and adolescents require different approaches. How is this factored in to The Shared Table program?
The Shared Table training focuses on the fundamental concepts of meal support which are valid across all age groups. At time of registration carers can select Supportive Meal Therapy Training for Carers (whose loved one is not engaged in Family Based Therapy); or Supportive Meal Therapy Training for Carers (whose loved one is currently engaged in Family Based Therapy).
The Shared Table program includes helpful accompanying written, video and audio resources providing tips and advice. This includes the 6 Cs: be calm, consistent and compassionate, show confidence, try coaching and don’t collude. How can families and support people deal with situations of extreme distress?
Carers and key support people are encouraged to contact EDQ to engage in carer coaching, to tailor skills and strategies from The Shared Table training to their personal situation. Carers must be residents of Queensland for eligibility for carer coaching. If a loved one is currently engaged in treatment, we strongly encourage the carer to advise the treatment team that they are completing this training. It is important to note that this training is not intended to replace any advice provided specifically to the carer and their loved one by the treating team.
Your work is based on Professor Janet Treasure’s evidence-informed, collaborative, skills-based approach involving families. How is this represented in the Shared Table program? What support is available for families having difficulties with Family-Based Therapy (FBT)?
The Shared Table is based on the fundamental concepts of supportive meal therapy, with strategies consistent with the approaches outlined by Professor Janet Treasure. EDQ’s Fostering Recovery Workshop is also based on the work of Professor Janet Treasure, and carers and key support people (who are residents of Queensland) are encouraged to engage in this workshop, to further increase their confidence and skills in providing meal support for their loved one/s. At time of registration for The Shared Table, carers can select Supportive Meal Therapy Training for Carers (whose loved one is currently engaged in Family Based Therapy). Carers and key support people are also encouraged to contact EDQ to engage in carer coaching, to tailor skills and strategies to their personal situation. Carers must be residents of Queensland for eligibility for carer coaching.
To access the Shared Table Carer Training Program, click here.
Melissa is the Senior Carer and Family Coach at Eating Disorders Queensland and is a registered Psychologist with the Psychology Board of Australia. Melissa has worked in the field of mental health for the past 11 years supporting children, adolescents, adults and families with a variety of mental health issues including eating and body image issues. Melissa’s approach is strengths based and person centred. Melissa values that people are the experts in their own lives and aims to collaboratively work with carers and key support people to provide them with the skills and knowledge they desire to support their loved one/s. Melissa is passionate about empowering carers and has seen the positive impacts this can have on supporting individuals through their recovery journey.
CEED, FYI and ROAR – Michelle Roberton
Accredited Practising Dietitian Michelle Roberton is Manager and Senior Clinician at the Victorian Centre of Excellence in Eating Disorders (CEED). She spoke with us about Feed Your Instinct (FYI) and Reach out and Recover (ROAR ), interactive online tools developed by CEED for parents and adults with eating and body image concerns respectively. Both tools generate reports, one tailored for the person and the other suitable for presentation to a GP or health professional to help communicate concerns.
You are an Accredited Practising Dietitian with more than 30 years’ experience in mental health. How did you become involved in the eating disorders sector?
It was rather a long time ago, but I got involved in the sector by happenstance really. I was appointed to one of a number of newly created dietitian positions in the then mental health hospital system in Victoria in the mid-80s. By chance the hospital I was appointed to, Larundel Psychiatric Hospital, happened to have an eating disorders unit. The team there welcomed me with open arms, and it has been an abiding interest ever since. Having a career as a dietitian, both in broader mental health and eating disorders, has given me the privilege of seeing the sector develop and emerge. In particular, I would like to note the increasing collaboration between people with lived experience, their supports and families and clinical services as a key approach to care and recovery. Through the COVID period and beyond, a demanding and exciting time is ahead of us all.
Feed Your Instinct (FYI) is an online tool created by CEED to help parents identify if their child has an eating disorder and support them to help their child recover. Tell us about the development of this program. How do you recommend parents use it?
In 2015, as part of the Victorian Government’s Eating Disorders Strategy 2014, CEED was given project funding focused on early intervention in eating disorders. FYI and ROAR online tools represented our strategy to promote early help seeking and action for change. The project involved surveying experienced carers/parents, expert parent focus and advisory groups, working with CEED clinicians and a carer consultant through all stages of development of the online tool. FYI was the first help-seeking promotion online resource for parents developed internationally.
Feed your instinct is a resource for parents who are becoming concerned about their child’s eating behaviour or body image worries. The FYI check list helps parents to understand that the concerns they have about their child’s eating and body worries are worth acting on. The responses to the checklist are created into a personalised report which can be used in discussion with their GP, and actions they can start taking right away to help their child at home. It has resources to guide GPs about physical risk and appropriate response and the importance of early referral to mental health eating disorders treatment and support.
Reach Out And Recover (ROAR) is an interactive tool designed by CEED to support people with body image and eating concerns to understand more about help-seeking and pathways to recovery. Tell us about the development of this program. How do you recommend people use it?
Part of the same funding program as FYI (mentioned above), ROAR online tools represented our strategy to promote early help seeking and action for change. Based on surveying and interviews with experts by consumer lived experience and advice and support from eating disorder sector experts by profession, the CEED team developed ROAR.
ROAR is aimed at fast-tracking help seeking in adults who have concerns about their relationship with food, nutrition, weight or exercise. ROAR uses a motivational enhancement approach to empower and encourage adults who have early signs of concern or with longer-standing eating disorders to take action to seek help and support.
ROAR utilises components of eating disorders/body image concerns and validated psychometric tools to formulate both a tailored personal report promoting self-efficacy and help seeking, and a tailored health professional report to support initial discussion with a GP or other health professional. ROAR also features psycho-education, including information about eating disorders including risks, the benefits of seeking help early, warning signs, treatment options including self-help options, and first contact and high-risk contact options. There are also personal stories of the recovery journey of a range of people who have experienced eating and body image problems.
These programs have been in place for four years. What has CEED learned over this time from participants? Have there been changes in the way people respond to these tools? Is there anything you would like to add?
We have seen an increased usage of both websites/online tools over these years. In particular, there has been a marked increase in accessing the tools over the extended COVID period which aligns with increased eating/body image and mental health concerns in the Australian community over this time period. The usage trends provide vital information about public demand and interest.
*Note: FYI usage trends illustrated in Figure 1 below show 5000 people visited the site in 2020-2021 (compared with fewer than 2000 in 2018-2019), and GP and parent report downloads increased by approximately a third in 2020-2021 from the previous financial year. ROAR usage trends illustrated in the Figure 2 below showed around 6500 people visited the site in 2020-2021 (compared with fewer than 1000 in 2018-2019), and visitors and GP and parent report downloads tripled in 2020-2021 from the previous financial year.
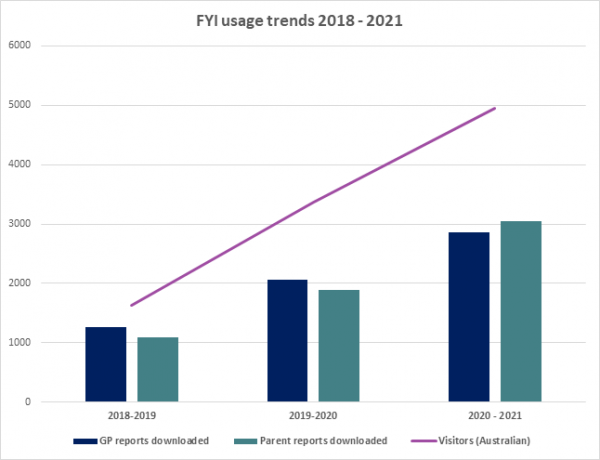
Figure 1: FYI usage trends over the four-year period since the introduction of the FYI program in 2018.
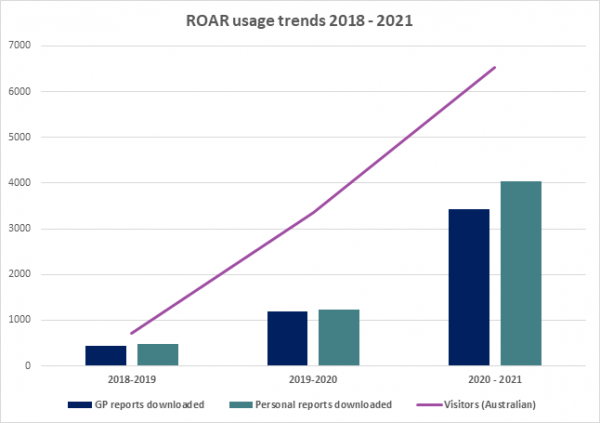
Figure 2: ROAR usage trends over the four-year period since the introduction of the ROAR program in 2018.
Early intervention is key to improving health and quality of life for people experiencing eating disorders. Beside FYI and ROAR, what other strategies or programs do you find useful?
Eating disorders and mental health support and information services are a vital resource to support those seeking help for the first time or having the courage to reach out again to find the help that is right for them.
Helpline services The Butterfly Foundation and Eating Disorders Victoria tell us they commonly use ROAR and FYI as part of their information hub/help line support resources. In the future we hope to ensure FYI and ROAR become one important help-seeking step that directly connects users to eating disorders service and system navigation support, and to e-support and treatment services.
To access Feed Your Instinct (FYI), click here.
To access Reach Out and Recover (ROAR), click here.

Michelle Roberton is an accredited practising dietitian (APD) and the Manager of the Victorian Centre of Excellence in Eating Disorders (CEED). Michelle has extensive experience in eating disorders and mental health in the public and private sector in a wide range of treatment, training and service development roles. As Manager at CEED, Michelle leads a multidisciplinary team of clinicians to collaborate with and support the Victorian health system to provide quality community treatment for eating disorders through service development support, clinical case consultation and workforce development.
Butterfly Foundation, Body Kind – Helen Bird
Helen Bird, Manager Education Services, Butterfly Foundation, spoke to us about the impact of COVID-19 on eating disorder services, addressing body image issues in boys and her organisation’s newest initiative, Body Kind Schools and Body Kind Families.
The COVID-19 pandemic has put mental health and eating disorders in the spotlight, with increasing numbers of young people trying to access services. How can Body Kind help schools and families address body image concerns and support the early identification of body dissatisfaction and eating disorders?
It certainly has been a challenging time. Butterfly Education Services have seen a significant spike in enquiries from schools due to the increased prevalence of body image concerns and eating disorders among students. How we work to prevent eating disorders is still very much being understood. However, there is evidence to support prevention approaches which focus on the known risk and protective factors that underpin the development of body dissatisfaction and disordered eating behaviours. Increasing understanding of these factors underpins all the education programs and resources at Butterfly, including Body Kind, our annual body image awareness initiative that runs every September.
Body Kind is about creating environments which support positive body image for young Australians. It specifically asks young people to be kind to their body and to others; kind in the language they use when speaking about bodies (face to face and online) and in the ways they move, nourish and nurture their bodies. Body Kind Schools (rebranded from Love Your Body Week for Schools in 2021) is an opportunity for education and youth organisations Australia-wide to come together and focus on these issues. Importantly, it’s been providing all those working with young people with free, evidence-informed and strength-based resources since 2017. This year we have over 1,600 schools/organisations registered with an estimated reach of over 200,000 young people.
Body Kind Families is a new initiative for 2021 and is a partner program to Body Kind Schools, extending the body kind messaging to the family environment. Body Kind Families is designed for parents of teenagers to help them better understand body image so they can talk to and support the teenager in their life with theirs. While it might not always feel like it, parents can still positively influence how their teen feels about their body and the behaviours they engage in. Body Kind Families also includes information on warning signs and what to do if your teen is struggling; the important message being to trust your instincts and intervene early.
Tell us about some of the downloadable and interactive resources included in the Body Kind program. How were they designed? How can schools and families use them?
Body Kind Families includes a range of bite-sized videos covering a range of topics to help parents understand what body image is and what influences it, particularly during adolescence - building resilience to media pressures, encouraging healthy eating and exercise behaviours, reducing appearance talk, being kind and compassionate to our bodies, and valuing and respecting all bodies. Each video is accompanied by a tips-sheet in print and audio format. There are also activities. For example, families might want to get involved in 30 days of Being Body Kind or use the Let’s Talk Being Body Kind Discussion deck to build connection and have an open discussion around body image. All of the content is designed to boost parents’ confidence to make positive changes, initiate conversations and respond in helpful ways and is based around the things that parents told us were important to them when we conducted a needs analysis at the beginning of the development process.
Body Kind Schools is similar in that it too provides free, evidence-informed resources including educator or peer-led workshops and classroom activities; fundraising ideas, posters, digital clips and support webinars, all aimed at those working in schools and other youth settings.
There is a simple registration process (so Butterfly can track uptake) to access resources for both initiatives and then it is up to schools and families to use the resources in a way that works best for them.
How have eating disorder experts and people with lived experience been involved in creating these resources and informing the development of the programs?
Thanks to the funding from nib foundation we were able to work with a range of leading body image experts to develop the video content for Body Kind Families and we are very grateful for the contributions of Dr Zali Yager, Louise Adams, Dr Fiona Willer, Alannah Dobson, Dr Jasmine Fardouly and Suzie Rhydderch.
The Butterfly Collective, our lived experience community were also involved early on and in reviewing draft content alongside our Parent and Stakeholder Reference groups.
Body Kind Families is aimed at parents and carers of teenagers. What about families with younger children? Do you have any practical tips?
While the content of Body Kind Families would be of interest to anyone wanting to understand more about body image there is specific content for families with younger children available through Butterfly’s Body Bright Program, a new whole of primary school body image program. In addition to the resources for families, Body Bright includes online staff training modules, curriculum-aligned lesson plans from foundation to year 6 and school culture guidelines.
In terms of tips, parents can aim to be a Body Kind role model by:
- Speaking kindly about their own bodies and all bodies
- Moving their body for health and wellbeing (instead of weight, body shape or muscle size)
- Expressing gratitude for what their body has done for them and what it can do
- Being aware of weight and appearance biases and challenging these
- Practicing self-compassion and self-care in a way that works for them
- Celebrating differences and non-appearance based qualities and achievements.
In addition:
- Embrace your child’s changing body and do your very best not to comment on their weight or body shape changes
- All bodies are different, support your child to accept their body more and compare less by seeing themselves as a whole person with passions, interests and hobbies, rather than focusing on appearance or body parts; and
- Help your child be body confident and kind on social media by encouraging authentic posting and developing their media literacy skills.
Body image concerns, muscle dysmorphia and eating disorders affect men and boys. How does Body Kind Schools and Families address issues affecting males?
Absolutely, there is growing evidence to suggest that males also experience anxiety about their body and appearance, which is why we developed RESET - a conversation about boys’ body image. RESET was designed in consultation with boys and leading mental health and body image experts and consists of a 30-minute video and facilitator guide to raise awareness, reduce stigma and encourage help-seeking. Designed for use in school and community settings, RESET is offered as part of Body Kind Schools, and alongside guidance on how it might be used in the home, it’s also available on the Body Kind Families resources page. Additionally, all Body Kind Schools and Body Kind Families content speaks to and is inclusive of all genders.
To access Body Kind Schools, click here.
To access Body Kind Families, click here.

Helen Bird has over 26 years of experience working in young people’s health promotion both at a policy and service delivery level in the UK and Australia. She has worked as part of Butterfly’s Prevention Services Team for over 7 years managing the delivery of specialised presentations, workshops and awareness initiatives in schools and community settings.
InsideOut Insititute, SupportED – Danielle Maloney
Danielle Maloney, Deputy Director of the InsideOut Institute for Eating Disorders, spoke to us about SupportED: Online Self-Help Program for Carers of People with an Eating Disorder, the recently launched Australian Eating Disorder Research and Translation Strategy 2021-2031 and the Top 10 Research and Translation Priorities.
It can be very difficult for people to find resources and encouragement to educate and assist them in supporting a loved one living with an eating disorder. How can Support ED help? How is it structured?
SupportED is an online knowledge and skills-based program for those who support someone with an eating disorder. The content of the program was developed by InsideOut Institute, in collaboration with Butterfly Foundation, EDFA, EDQ and EDV, with significant involvement from those with lived experience and expert clinicians.
The program is very grounded in practical skills and resources. Presented over five modules, while we have included information about eating disorders and their treatment, the main part of the program focuses on skills identified to facilitate them in their support role including: communication skills, practical skills, dealing with risk and comorbidities, how to facilitate recovery and how to manage emotions and burnout.
Participants can choose to do all five modules or just the sections that they find most relevant. The program also helps to navigate currently available resources which carers may find helpful from a variety of organisations (over 200 different resources at last count).
What skills, knowledge and resources are important for families and supports of people living with an eating disorder? How is this presented in InsideOut’s online program?
We surveyed and interviewed over 100 people with lived experience of an eating disorder and/or of providing support. They told us they wanted easy to access information on hand for when they needed it, practical advice and to hear from others who had been in their position.
Particularly families and supports wanted to know more about strategies for mealtimes, dealing with times of conflict, transitioning between services and home from inpatient admissions, finding the right treatment and talking to treatment teams, knowing where and how to access support (practically, psychologically and financially).
SupportED includes written information, instructional role plays and animations to really demonstrate these practical skills. There are also videos of clinicians providing expert advice, alongside the experts there are videos and audio from those with lived experience of an eating disorder and of providing support who give tips and information from their own journeys.
Negotiating mealtimes, dealing with conflict and coping with burnout can affect a person’s ability to continue their supportive role with confidence. How are these issues addressed in the program?
These real-life challenges - conflict, burnout and mealtimes - came up frequently in consultation with carer groups as well as in the research literature. The program covers each of these challenges in order to build the confidence of the participants to deal with them.
We know that having support around meals is key for someone with an eating disorder as it helps them to manage and decrease their distress. Support people can play a key role at mealtimes. Meal support involves providing emotional support, encouragement and reassurance before, during and after meals. SupportED provides practical strategies for before, during and after mealtimes and links to additional resources and skills-training.
When it comes to conflict, it is normal for debate, negotiation and disagreements to occur as those with lived experience navigate the road to recovery with their loved ones. These discussions will often be necessary and important; however, it is important for support people to know how to avoid hostilities and significant conflict where possible. The program includes tips for avoiding conflict where possible and practical advice on how to de-escalate challenging situations when conflict does occur.
Research suggests that to reduce burnout it is important that support people have available basic information about eating disorders including treatment options; have skills/strategies that work and that they are actively working on caring for themselves during this process. Self-care strategies are dispersed throughout the program. We firmly believe that carers need care too.
Online programs have different requirements and possibilities to face-to-face programs, which have been made increasingly inaccessible due to COVID-19. How is SupportED different to conventional programs?
Targeted educational and practical skill-based programs have been found to improve coping, knowledge, communication and overall skills resulting in reduced stress and burden.
Many skills-based programs have been offered face-to-face and via video link and can be very successful; however, these are often time limited, only available to those in certain geographical locations or sometimes to a subset of carers (for example, parents of someone with anorexia nervosa), thereby limiting accessibility.
Prior to the development of this program there was no routinely available continuous skill-based programs online or face-to-face in Australia. An online continuously available program allows participants to work through the content at their own pace, at a time that suits them from their own home and to go back over things they want to review.
In addition to knowledge and skills, as we know carers can significantly benefit from support groups and peer mentoring, where there is an opportunity to share their experiences and emotions with others who have had similar experiences. While this isn’t possible to be offered as part of SupportED, the program addresses this need by having content which is interspersed with lived experience quotes and videos. Participants are also encouraged to connect with other carers through available programs (such as groups offered by The Butterfly Foundation and Eating Disorders Families Australia).
The program also provides practical steps to help support people to communicate with their loved one’s treating team for specific/individualised information and advice, and to seek their own support whether that be practical, financial or for their own mental health.
SupportED is particularly interesting as people taking part are also participating in a research study evaluating the program itself. What does the study involve? How does the study component of SupportED work with the program to improve its content, delivery, and future development?
As this is a new online training program, prior to releasing it as an ongoing program, it was very important to evaluate it to determine the program’s effectiveness.
Participation in this research study is voluntary and will provide support people with access to SupportED for an initial three months, free of cost. Participation in the study involves completing brief questionnaires at the beginning of the program, end of the program and three months after completing the program. We also invite participants to provide us with further feedback via a Zoom or phone-based follow-up interview.
This valuable feedback will allow us to understand how support people interact with the online nature of the program and to continue to adapt the content, and delivery of the program to better meet the needs of carers into the future. Feedback in the past 6 months has been overwhelmingly positive and we expect to start formally publishing outcome data over the next 12 months.
This will add to the literature in the field and has the potential to influence clinical practice for the better, and ultimately improve accessibility to this type of program.
InsideOut launched their Australian Eating Disorder Research and Translation Strategy 2021-2031 in September, including the Top 10 priorities. Tell us about this initiative and the pivotal role of research.
We have said this often at InsideOut, but it truly takes a village. The Australian Eating Disorder Research and Translation Strategy 2021-2031 is the culmination of a truly national process involving the active participation of over 480 individuals consulted, representing 80 different organisations, our lived experience research advisory group, and our national expert research collaboration.
This is a significant milestone for the eating disorder community as it is the first Australian disorder-specific mental health research and translation strategy. It is also critically important as investment for eating disorder research per affected individual in Australia to date is significantly less than for autism, schizophrenia or the depressive illnesses, despite comparable illness and cost burden. This needs to change, and the Strategy calls for actions that will drive that change.
The Top 10 priorities were developed in a wholly co-designed process. This process acknowledges that it is the priorities and needs of the people who are most impacted by research that should guide the research that is funded and conducted. The 10 research priorities identified in the Strategy cover the areas of prevention, risk and protective factors, early identification, equity of access, treatment outcomes, individualised medicine, family support, early intervention, positive and negative treatment impacts, stigma and health promotion.
This is the start of the conversation that we need to have nationally. Strengthening eating disorder research and translation in Australia will ensure that we find and deliver the latest and best possible support for those impacted and their families and carers. It will lead to significant improvements in the wellbeing of people at risk of or living with an eating disorder and, most importantly, will save lives.
For more information about SupportED, please watch this five-minute video here.
To access SupportED, click here.

Danielle Maloney is the Deputy Director of the InsideOut Institute – Australia’s first institute for research and clinical excellence in eating disorders. She is also head of the Service Development and Policy team. She holds an Honours degree in Psychology, a Master’s degree in Public Health and an International Master’s of Mental Health Policy and Services. Danielle has more than two decades of experience in public health, the last 20 years of which she has spent working in the mental health sector. Danielle has spearheaded the development of new and innovative health programs particularly in the child and adolescent mental health space, and more recently in eating disorders, and has overseen the roll out of large-scale clinical training programs. She has recently, with her team, written the NSW Service Plan for People with Eating Disorders 2021-2025 and oversaw the development of the Australian Eating Disorders Research & Translation Strategy 2021-2031.





