People experiencing an eating disorder can access treatment through either an Eating Disorder Treatment and Management Plan (EDP), Mental Health Care Plan, and/or Chronic Disease Management Plan.
This page provides information for people seeking treatment for an eating disorder and for health professionals. It outlines the treatment and services available under an EDP, including the practitioners involved, the steps involved in developing an EDP, and links to Medicare Benefits Schedule (MBS) items.
What is an EDP?
On 1 November 2019, the Australian Government introduced a suite of new MBS items for people living with anorexia nervosa and other eating disorders. The changes are relevant for medical practitioners (including GPs, psychiatrists, and paediatricians), and eligible psychologists, occupational therapists, social workers, and dietitians. The information on this page is sourced from the Quick Reference Guide for Eating Disorder MBS items and Services Australia's eating disorder treatment and management plans webpage.
People eligible for the EDP are able to access comprehensive treatment and management services for a 12-month period, including:
- assessment and treatment planning
- up to 40 sessions of evidence-based psychological treatment from a mental health professional. This can include individual and/or group sessions.
- up to 20 sessions of dietetic services from an Accredited Practicing Dietitian (as recognised by Dietitians Australia)
- review and ongoing management services to ensure the person accesses the appropriate level of intervention
Who is eligible for an EDP?
There are two cohorts of eligible patients who can access EDPs:
- People with a clinical diagnosis of anorexia nervosa; or
- People who meet the eligibility criteria (below) and have a clinical diagnosis of bulimia nervosa, binge eating disorder (BED) or other specified feeding and eating disorders (OSFED).
People living with anorexia nervosa are eligible for an EDP without any further criteria needing to be met.
The eligibility criteria that need to be met for a person with a clinical diagnosis of bulimia nervosa, BED and OSFED, are:
- Eating Disorder Examination Questionnaire (EDE-Q) scores ≥ 3 and
- The condition is characterised by rapid weight loss, or frequent binge eating, or inappropriate compensatory behaviour as manifested by 3 or more occurrences per week and
- Two of the following indicators are present:
- clinically underweight with a body weight less than 85% of expected weight where weight loss is directly attributable to the eating disorder
- current or high risk of medical complications due to eating disorder behaviours and symptoms
- significant functional impairment resulting from serious comorbid medical or psychological conditions
- admission to a hospital for an eating disorder in the previous 12 months
- inadequate treatment response to evidence-based eating disorder treatment over the past 6 months despite active and consistent participation.
Developing an EDP
A medical practitioner in general practice (e.g., GP), consultant paediatrician, or consultant psychiatrist can develop an EDP. This practitioner is recognised as the managing practitioner. It is important to allow a longer appointment time to discuss and develop a plan that meets the needs of the person living with an eating disorder.
The EDP needs to include:
• opinion on diagnosis of the person’s eating disorder
• treatment options, goals, and recommendations
• referrals to allied health professionals for mental health and dietetic services, and specialists, as required, for the 12-month period.
It is important that the referring medical practitioner, mental health and dietetic treatment providers, and the person living with an eating disorder have a copy of the plan. With permission from the person living with an eating disorder, a copy should also be offered to identified support people, such as family.
The managing practitioner will make referrals to a mental health professional and a dietitian. Mental health professionals able to provide treatment under an EDP include eligible psychologists, occupational therapists, social workers, and medical practitioners in general practice with appropriate mental health training. Costs and rebates for sessions will vary depending on which professional is providing the treatment.
To create an EDP for an eligible person, the medical practitioner can use the InsideOut Institute Eating Disorders Care Plan template.
Psychological treatments approved for use by practitioners providing psychological treatments under an EDP
It is expected that practitioners who are providing services under these items have appropriate training, skills, and experience in treatment of people with eating disorders and meet the national workforce core competencies for the safe and effective identification of and response to eating disorders. More information here.
The following treatments have been approved for use under an EDP:
• Family Based Treatment (FBT) for Eating Disorders (including whole family, Parent Based Therapy, parent only or separated therapy)
• Adolescent Focused Therapy (AFT) for Eating Disorders
• Cognitive Behavioural Therapy (CBT) for Eating Disorders (CBT-ED)
• CBT-Anorexia Nervosa (CBT-AN)
• CBT for Bulimia Nervosa and Binge Eating Disorder (CBT-BN and CBT-BED)
• Specialist Supportive Clinical Management (SSCM)
• Maudsley Model of Anorexia Treatment in Adults (MANTRA)
• Interpersonal Therapy (IPT) for Bulimia Nervosa and Binge Eating Disorder
• Dialectical Behavioural Therapy (DBT) for Bulimia Nervosa and Binge Eating Disorder
• Focal Psychodynamic Therapy for Eating Disorders
Duration of an EDP
An EDP is valid for 12 months from the date the EDP was created by the medical practitioner and not based on a calendar year. The person’s count of EDP psychological and dietetic services should start from the date of the EDP and apply to all services provided within that 12-month period.
Once this time has lapsed, a new EDP will need to be created and new referrals made for psychological and dietetic treatment. Sessions that were not used in the preceding 12 months cannot be carried over into the new plan. If the 40 psychological and/or 20 dietetic sessions are used in under a 12 month-period, the person will need to wait until the 12-month period has lapsed before accessing further sessions under a new EDP if eligible.
NOTE: If a person commences a second EDP, the specific time of the year that the person accessed the psychological and/or dietetic sessions during the 12 months of the first EDP does not impact on accessibility of sessions in the subsequent EDP plan. For example, if most of the psychological sessions are accessed in the final quarter of EDP #1, the psychological sessions in EDP #2 can be accessed when they are required and not based on a rolling year calculation.
Reviews and referrals within an EDP year
The managing practitioner is expected to review the person on a regular, ongoing and as required basis and will manage the reviews needed for the person to utilise an EDP. This should occur in addition to regular medical monitoring by a medical practitioner. The reviews and medical management can be provided by the same medical practitioner.
A review is required by the managing medical practitioner after every 10 mental health sessions. This means that a review of the EDP by the managing practitioner may be required up to 3 times over the 12-month period.
A specialist review by a psychiatrist or paediatrician is required for the person experiencing an eating disorder to be able to access the additional 20 psychological sessions. This review can occur at any point before the 20th psychological session. The managing practitioner should make a referral for specialist review as early in the treatment process as appropriate. See below for a flowchart of the steps involved in accessing the services under an EDP.
This Session Planner can help to track sessions and review points within the EDP. It is relevant for the managing practitioner, treatment providers, and person experiencing an eating disorder.
Case conferences
Case conferences can be held for people who have an active EDP. Case conferences must be organised by the medical practitioner (GP, consultant physician in their specialty of paediatrics or psychiatry) and involve at least two other members of the multidisciplinary care team providing different types of treatment to the person. The person, family members, carers, or other people providing support to the person experiencing an eating disorder can attend the case conference, but do not count towards the minimum number of providers required.
It is expected that a person experiencing an eating disorder would not require more than four case conferences within a 12 month period.
Further information about case conferences within an EDP can be found on MBS Online.
EDPs and other care plans
People living with an eating disorder may have more than one care plan in place, and services under other care plans count towards the total services a person can have under their EDP. If someone is accessing care under a Mental Health Treatment Plan (see below) or a Chronic Disease Management Plan, it is essential that these mental health and/or dietetic sessions are included in the total number of mental health and dietetic sessions accessed under the EDP.
If a person is experiencing comorbid mental health difficulties in addition to an eating disorder, treatment for this comorbid mental health condition should occur under the EDP psychological treatment services. If a person has an EDP in place, the development or review of a Mental Health Care Plan should not occur unless there are exceptional circumstances. See page 190 of the full Medicare Benefits Schedule Book for further information.
Please see Medicare items webpage for more information about Mental Health Care Plans and Chronic Disease Management Plans.
MBS Items
An EDP is developed by a GP or medical practitioner (items 90250-90257), consultant psychiatrist (items 90260-90262) or consultant paediatrician (items 90261-90263). See the MBS Quick Reference Guide for more information.
The full Medicare Schedule Book can be accessed online. Content relating to eating disorders can be found in the following sections:
• Pages 183-196 - General explanatory notes, patient eligibility, overview of items, EDE-Q, telehealth, requirements for medical practitioners in the development and review of EDPs, requirements for provision of psychological treatment services
• Pages 346-359 - Item specific information for GPs and other Medical Practitioners
• Pages 1378-1394 - Item specific information for Dietitians
• Pages 1378-1383 - Psychologists
• Pages 1384-1386 - Occupational Therapists
• Pages 1386-1389 - Social Workers
Treatment under an EDP - Flowchart
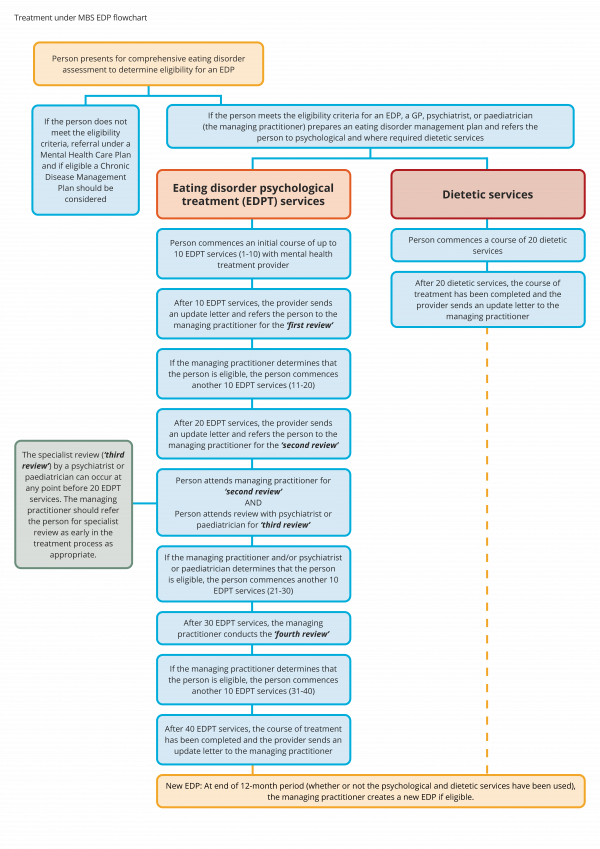
Click here to download.
July 2021 changes
Commencing 13 March 2020 and extending until 31 December 2021, the Australian Government made a number of temporary MBS telehealth (video and telephone) items available to help reduce the risk of community transmission of COVID-19 and provide protection for people experiencing eating disorders and health care providers. From 1 July 2021, GP and Other Medical Practitioner telephone items were be streamlined. This change aligns with how the items are being used by providers and is also based on expert advice about the use of telephone-based services.
No changes to face-to-face items or telehealth items delivered via videoconference have been made.
Click here to access a fact sheet produced by NEDC containing information about the new, continuing and discontinued telephone items from 1 July 2021, which may be relevant to GPs and Other Medical Practitioners providing services via telephone to patients experiencing an eating disorder.
Evaluation of the Eating Disorder MBS Items
Read our summary of the evaluation of the 2024 Eating Disorder MBS items here.
Further information and support
A joint response from Butterfly Foundation, NEDC, and the Australia and New Zealand Academy for Eating Disorders (ANZAED) addressing Frequently Asked Questions is available here.
The Butterfly Foundation provides comprehensive information about how to access an EDP through your GP, the steps involved, and finding a mental health professional able to provide treatment.
For further information on eligibility criteria, including using the Eating Disorder Examination Questionnaire and indictors, see Services Australia and MBS Online.
See the panel on the right of this page for links to useful forms and further information.

